Global health leaders are confronting a new reality: Multilateral aid is contracting, major donors are pulling back, and low- or middle-income countries—particularly in Africa—are forced to tackle more complex, frequent, and widespread health threats with fewer resources. As health systems grapple with growing pressure and unpredictability, the need for locally driven, sustainable solutions is becoming ever more urgent.
That's why, with regional manufacturing high on the agenda at the Group of 20 (G20) Health Working Group last week in South Africa, global attention is turning to a truth many countries in Africa have long recognized: Health security cannot depend on distant suppliers and uncertain aid. This moment demands not only reflection, but also reinvention.
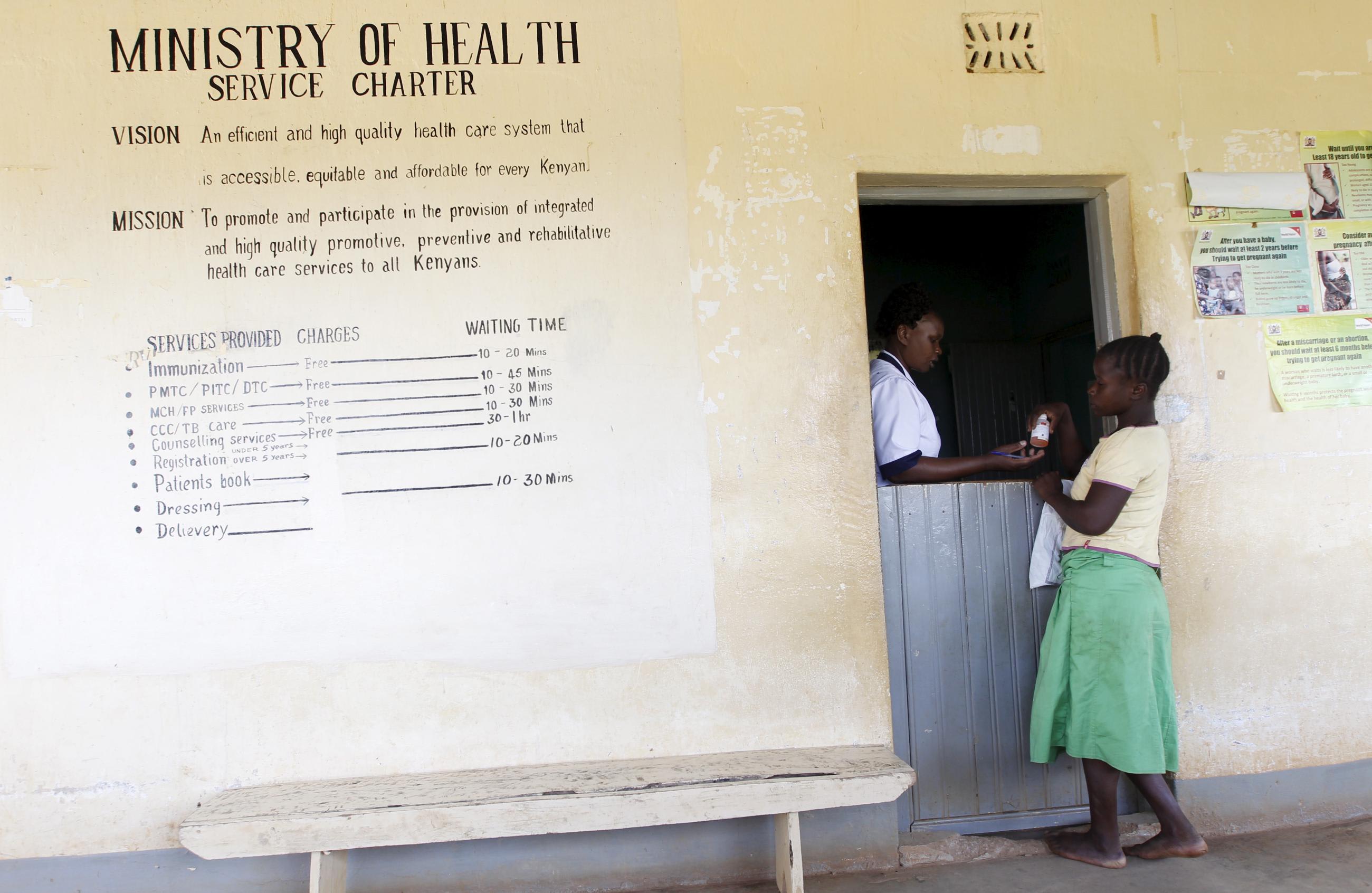
Nowhere is this need more urgent than in the production of health products. Africa bears 25% of the global disease burden—including major infectious diseases such as HIV, tuberculosis, and malaria—yet it imports more than 95% of the active pharmaceutical ingredients and 70% of the medicines it consumes [PDF]. This leaves countries vulnerable to supply-chain disruptions, price shocks, and unpredictable donor shifts. Patients who rely on steady access to quality-assured tests and treatments are already seeing devastating consequences.
To understand the scale of the challenge, consider this: Africa is home to 1.5 billion people but has just 600 health-product manufacturing sites. In contrast, India is home to 1.4 billion but has approximately 10,000 sites, and China has around 5,000 sites for a similar population. This vast disparity leaves African nations more exposed to global supply-chain shocks and limits their ability to respond to local health needs with the speed, affordability, and self-reliance needed to ensure essential products are available when and where they're needed without depending on distant suppliers or uncertain aid.
As health systems grapple with growing pressure and unpredictability, the need for locally driven, sustainable solutions is becoming ever more urgent
Here, autonomy refers to the ability of African countries to act independently and make timely decisions in addressing their health needs—without being overly dependent on external suppliers, donors, or complex global supply chains. The goal is to have enough self-reliance in manufacturing capacity, procurement systems, and regulatory oversight to ensure essential health products are available when and where they're needed.
As more countries move away from aid dependency, Nigeria is demonstrating how political will, smart investment, and regulatory reform can begin to reshape the health manufacturing landscape.
Reducing Import Dependency
Across the continent, investment in local capacity for regional production of health products is growing, with more African countries now prioritizing it in national industries, science, and health strategies. Regional partnerships are emerging, investments in Africa are increasing, technology transfer is accelerating, and manufacturers on the continent are expanding their capacity.
As Africa's most populous country and the region's manufacturing anchor, Nigeria offers a glimpse of what's possible when commitment meets action. Home to nearly 60% of West Africa's pharmaceutical production capacity, Nigeria has stepped up local investment, with strong leadership from the highest levels. Last September, as part of the Presidential Initiative for Unlocking the Healthcare Value Chain (PVAC), the government signed an agreement with Vestergaard, a Swiss manufacturing company, to establish the continent's first manufacturing hub for dual-insecticide treated bed nets—a vital step in combating malaria and boosting regional supply-chain resilience.
Building on this momentum, Nigeria is strengthening its regulatory oversight through its National Agency for Food and Drug Administration and Control, which now requires studies to show that generic medicines work the same as brand-name versions—helping ensure they are safe, effective, and trusted in health-care settings. In April, the government announced that it seeks to increase local pharmaceutical and medical device manufacturing to meet 70% of domestic demand and contribute at least 15% of the continent's need by 2030.
Through those initiatives, Nigeria is positioning as a regional supplier and demonstrating how countries can reduce import dependence and build health systems that are both resilient and self-reliant.

Local Investment Projects
One of the most promising examples of this shift is Emzor Pharmaceuticals' $23 million investment in a new active pharmaceutical ingredient (API) production facility in Sagamu, Ogun State, Nigeria, that is set to begin operations later this year. APIs are the first step in the complex pharmaceutical supply chain. They are the ingredients that make medicines effective and are combined with other ingredients to become final products, such as tablets or capsules.
Today, nearly all of Africa's APIs come from outside the continent—mainly from China— and India dominates in producing the finished medicines shipped to African countries. Expected to begin operations in late 2025, the Emzor plant will help reduce Nigeria's reliance on imported raw materials and bolster its role as a regional manufacturing hub. This kind of investment is not just about local supply—it's about building capacity at the most critical stage of drug production.
Progress however, will only be sustained if it's matched by the right investments—not just in infrastructure, but in markets. African pharmaceutical manufacturers currently operate at just 30% to 60% of their production capacity relative to more than 70% in more developed economies in Europe and North America. Without reliable demand, even well-equipped factories struggle to stay viable. Manufacturers need confidence that their products will be purchased at sufficient scale to justify continued investment. African governments should lead this investment by procuring regionally made products, and development partners should reinforce that leadership with catalytic, demand-focused support.
Unitaid's work in Senegal showcases what this looks like in action. During the COVID-19 pandemic, Unitaid and FIND supported the expansion of diaTROPIX, a diagnostics facility at Institut Pasteur de Dakar, helping it scale up production from 1 million to 75 million tests per year. With technology transfer from partners in the United Kingdom and Korea, the facility began with COVID-19 tests in 2021 and later pivoted to blood-based HIV tests and other diagnostic tools as COVID-19 cases subsided. The expansion of the diaTROPIX facilty shows that flexible, regionally anchored manufacturing doesn't just serve short-term needs but also builds capacity to respond to enduring health threats.
This same method is being applied to other essential health products. In East Africa, Unitaid is partnering with CHAI, MedAccess, and Kenyan and Tanzanian gas companies through the East African Program on Oxygen Access to build sustainable, locally owned medical oxygen production infrastructure in Kenya and Tanzania. These facilities are designed not only to treat patients today, but also to ensure that the region can respond more quickly and more independently when the next crisis comes.
Development Actions to Meet the Moment
When countries are home to regional manufacturing hubs, they can produce health tools including oxygen, diagnostics, and medicines within integrated value chains—meaning that all stages of production, from sourcing raw materials and manufacturing components to assembling, quality control, and distribution, are connected and managed within the region. Those hubs strengthen regional supply chains that bolster countries' economies and allow them to better response to local needs. Turning this vision into reality, however, requires overcoming major hurdles that include high production costs, complex regulations, weak human capacity, limited financing, weak infrastructure, and uncertain demand.
Advancing regional manufacturing will take coordinated action—from governments to create an enabling environment with strong policies, infrastructure, and regulatory systems; from manufacturers to build strong partnerships for technology transfer; financing and product development; and from buyers to create stable demand by purchasing quality-assured products made on the continent.
Equally important is the role of civil society in advocating for transparency and equitable access to health products as well as ensuring that the voices of communities facing the greatest health inequities are heard. Leaders should also recognize the private sector's and faith-based organizations' contributions. As major providers of care in many African countries, these organizations are well positioned to expand access to regionally manufactured products, support last-mile delivery, and build trust in health innovations through their deep community ties. For this to succeed, governments, manufacturers, buyers, civil society, the private sector, and communities must all take part.
The moment demands these actions. The shift from dependency to resilience won't happen overnight but it is under way. As countries such as Nigeria pave the way, partners should follow with humility, alignment, and purpose.
African nations are not asking for permission to lead. They are already leading. Now, health systems, markets, and civil society need to keep that momentum going.