In a widely circulated white paper published in March, the Community Health Impact Coalition articulated priorities for the global COVID-19 response. We argued that community health workers—lay people who are trained to provide health services in their neighborhoods—are poised to play a pivotal role in fighting the pandemic and outlined the targeted actions needed at different stages of the pandemic to (i) protect health-care workers, (ii) interrupt the virus, (iii) maintain existing health-care services while surging their capacity, and (iv) shield the most vulnerable from socioeconomic shocks.
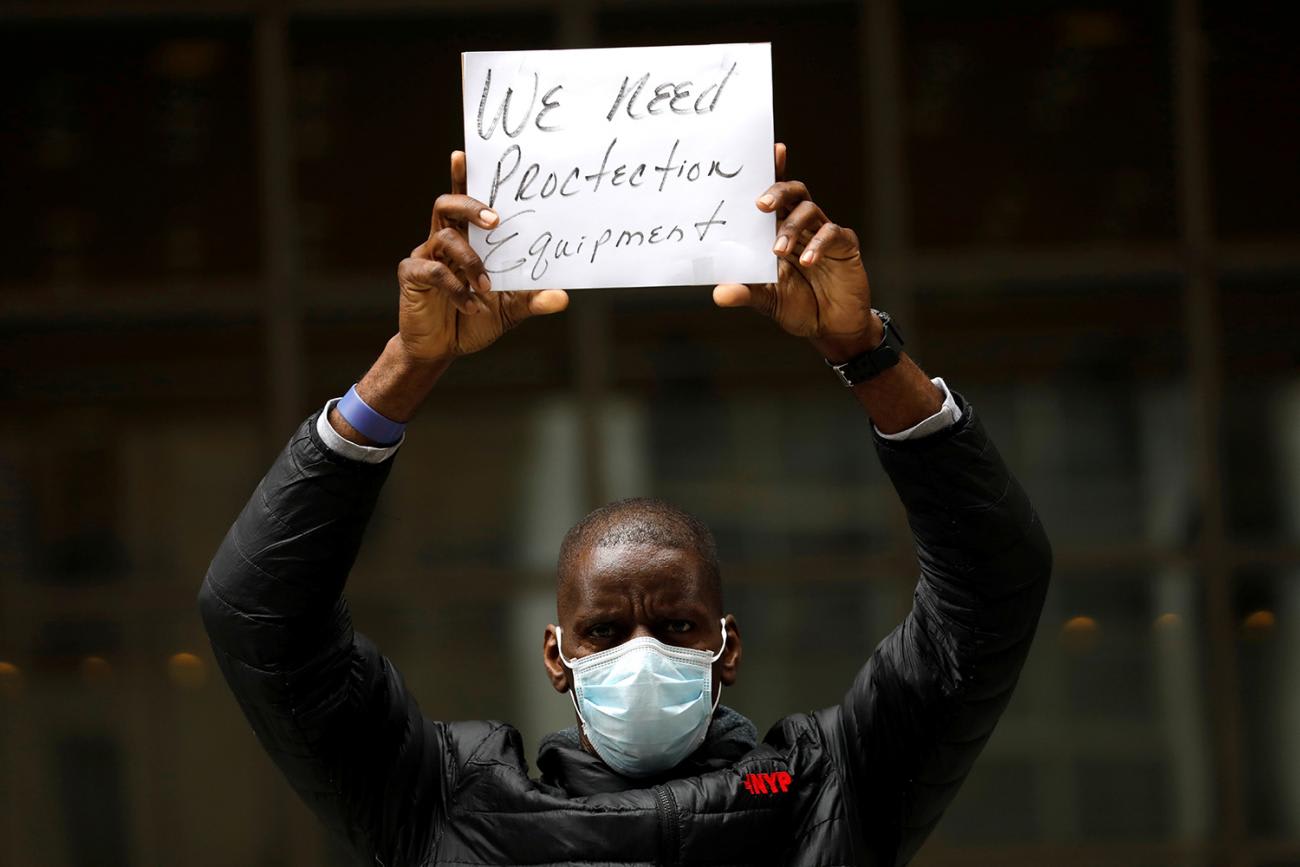
It is now clear that decisive action to blunt the impact of the pandemic in countries about to be hit the hardest is facing a critical bottleneck: community health workers—despite being a critical part of the response—are not receiving personal protective equipment (PPE).
COVID-19 spreads primarily through droplets emitted while coughing, sneezing, or even speaking. PPE (e.g., facemasks, goggles, gloves) is essential to keep health workers safe and prevent them from potentially spreading the disease to others. Without PPE, community health workers can neither maintain existing health services nor conduct the additional services required to interrupt and control the virus.
The collective failure to provide adequate PPE to community health workers in emerging COVID-19 hotspots will be catastrophic
Since the COVID-19 outbreak began, global demand for PPE has grown by a factor of twenty. While a global shortage of PPE is affecting all health workers, the brunt has fallen on low- and middle-income countries and community health workers in particular. In a time when every nation that has planked the curve has recruited community health workers to conduct aggressive community testing and contact tracing, the collective failure to provide adequate PPE to community health workers in emerging COVID-19 hotspots will be catastrophic. The alternatives are grim. community health workers in many countries are receiving instructions from the health system to either stay home, stop working, and cease providing essential health-care services to their communities—or keep working with no protection, putting themselves, their families, and the people they serve at risk.

COVID-19 is not over for anyone until it is over for everyone. Community health workers are ready for the fight, but they quickly need to be equipped with the proper quantity and quality of PPE.
Quantity: Counting the Uncounted
Community health workers cannot get PPE if they are not included in national planning and projections. Several countries have excluded or deprioritized community health workers in PPE projections because the "COVID-19 Critical Items" guidance from the World Health Organization (WHO) advises, "Priority for PPE provision is given to health-care workers treating critical and severe COVID-19 patients only."
This is a disconnect. Community health workers encounter the critically ill as part of their routine service delivery, and all it takes is one such encounter to get infected and potentially spread the infection to others. In fact, recent estimates indicate that 44 percent of secondary transmission could occur in presymptomatic patients.
For community health workers to continue to provide lifesaving care face to face, PPE is required
Without PPE, community health workers must attempt to treat patients from six feet away. For many services (e.g., malaria testing, immunizations, screening for malnutrition) this is impossible. Limiting the care community health workers provide also has the potential to increase the burden on health facilities with cases that could otherwise be managed at home. This additional pressure to already-stressed health systems places patients and other health cadres at further risk. For community health workers to continue to provide lifesaving care face to face, PPE is required. Critically, this is true of all community health workers—formal or informal. Although the WHO COVID-19 Essential Supplies Forecasting Tool used by many ministries of health to quantify PPE includes community health workers, its use of International Standard Classification of Occupations (ISCO) codes excludes the hundreds of thousands of hidden volunteer community health workers who do not meet the ISCO criteria but are nonetheless tasked with delivering health-care services in homes and communities.

Ministries and partners should therefore act quickly to adjust their PPE forecasts, effectively counting the uncounted so all community health workers can be equipped. If community health workers' rolls are inaccurate or nonexistent, funders, civil society, and norm-setting institutions should support ministries to make the best estimates possible of community health workers numbers, services, and distribution so that none are left behind.
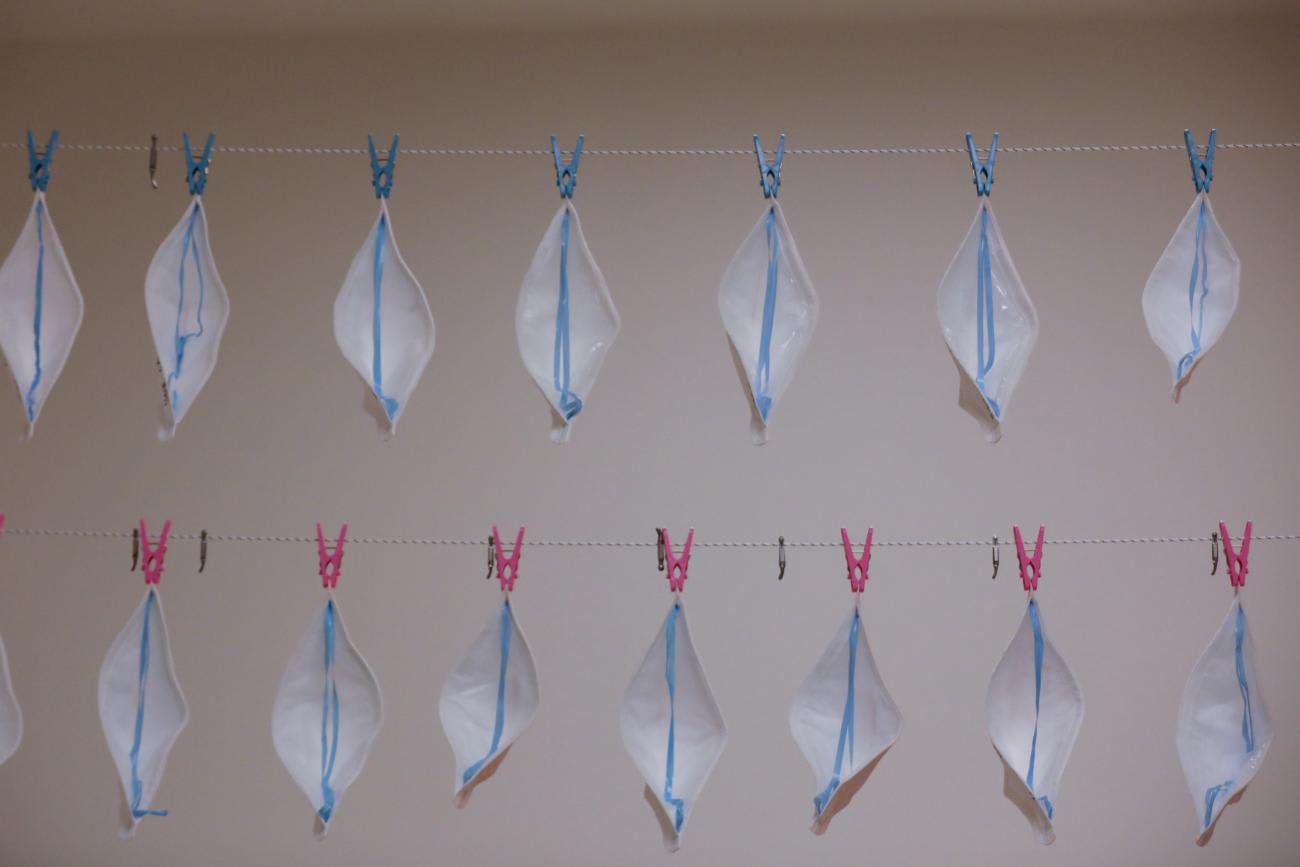
Quality: Same Standards for All
Not all PPE is the same, and community health workers deserve quality PPE just like any other health worker. Cloth masks, for example, are not equivalent to respirators (N95s) and surgical masks: rigorous studies show that cloth masks do not provide adequate protection for health-care workers, yet around the world community health workers are being asked to use them.
Community workers can be infected by COVID-19 as easily as any health-care worker, and in many ways they are even more vulnerable. They are more likely than their health facility–based counterparts to live in rural areas far from health facilities, have underlying conditions such as HIV/AIDS, or have less access to wash stations and sanitizer. They are clearly in need of protection, but we are not standing with them in this time of need.
Community health workers, like any health worker, ought to have the following:
- surgical masks—or N95 masks if performing aerosolizing procedures like nasal swabs;
- gloves for each patient encounter (or the ability to sanitize hands);
- eye protection; and
- disposable gowns (or ability to launder uniforms each day).
Time is quickly running out for these policies to be fully reversed
In the context of a global PPE shortage in which wealthier countries are outbidding low- and middle-income countries, supply must be increased and the playing field leveled. To address supply, governments should cultivate public-private partnerships with manufacturing and production companies. PPE export bans and restrictions on spending federal aid money on PPE that make it harder for those most in need to secure quality PPE must be eliminated. COVID-19 has been slow to spread in Africa, but a wave will soon hit. Time is quickly running out for these policies to be fully reversed. Without PPE, community health workers can neither maintain existing health services nor conduct the additional services required to interrupt and control the virus. Without PPE, we risk cutting essential health services and the health workforce off at the knees and putting community health workers and the people they serve at risk. As first responders in their communities, these workers are entitled to the same treatment as nurses, doctors, and other health providers. PPE allocation should depend on the service provided, not on the service provider.

Although governments and health systems are facing incredible challenges at this moment, achieving PPE for all is not only necessary, but possible.
- To address the global PPE shortage, governments should cultivate public-private partnerships with manufacturing and production companies to increase the global supply of PPE;
- To address inequity in PPE access between rich and poor countries, we must (i) end PPE export bans and restrictions on spending bilateral aid money on PPE and (ii) correctively include PPE for community health workers as a priority in multilateral, bilateral, and foundation funding strategies.
- To address the exclusion of community health workers from national projections, (i) global guidance should clearly and consistently articulate the need for these workers—formal and informal—to be included in PPE projections, and (ii) governments should count community health workers—formal and informal—and include them in projections and budgeting for PPE allocation.
None of us are safe until all health workers are protected. The time to start is now.












