President Donald J. Trump is one of the world's most powerful people, leader of its richest country, and now a part of the growing SARS-CoV-2 disease 2019 (COVID-19) morbidity statistics. He is the first U.S. president to have been hospitalized in over forty years, a fact that enshrines COVID-19 as a clear national security threat. This virus has overwhelmed the United States with more than seven million diagnosed cases and more than 200,000 reported deaths. This national tragedy has been magnified by poor policy choices and misaligned priorities. An all-too-familiar narrative, encompassing political ironies and constitutional crises, highlights the national security risks associated with underfunded public health and health-care infrastructures. Moreover, we can recognize that the current individualistic model for public health—that erroneously de-emphasizes social responsibility—will continue to fail the American people.
Chronically defunded public health sectors
President Trump's recent diagnosis positioned COVID-19 as a threat to national security. However, we should not ignore the fact that we were underprepared, and that the poor U.S. outcomes in the COVID-19 pandemic are partly the consequence of chronically defunded public health sectors, which is really the most fundamental risk to national security. The interplay between public health and national security is often discussed within the context of bioterrorism, but bad actors and rogue nations are only part of the threat. Emerging infections, like COVID-19, are bound to happen, and they presents an opportunity to reconsider the national security implications of strengthening public health infrastructure.

Investment Disparities: Public Health and Universal Health Care
Far too often, we are reminded that a chain is only as strong as its weakest link. The COVID-19 pandemic led to a near-collapse of our costly, inefficient health-care system and highlighted the inadequacies of our underfunded, fragmented public health infrastructure. Public health professions have warned audiences of such a scenario before. The U.S. decision to defund vital public health programs, such as the U.S. Agency for International Development's previously funded global effort to detect viruses in animal hosts with pandemic potential, was unfortunate. The failure to legislate a better health-care system that delivers comprehensive coverage to all, absent costly insurance premiums, high deductibles, and gaps in coverage, has turned out to be tragic. The novel coronavirus has laid bare how the U.S. now lacks the capacity to respond to a significant global public health crisis accordingly.
U.S. spending on health care is $11,172 per person—roughly 18 percent of GDP
The United States spends approximately $3.6 trillion or $11,172 per person each year on health care, accounting for roughly 18 percent of our gross domestic product. The United States currently ranks the highest in health-care spending globally. Inconsistently, only $19 per capita is spent on evidence-based public health initiatives, while at least $32 per person is actually needed to satisfy foundational public health service needs. Health-care spending as it exists in the United States is something of a fiscal armageddon—unsustainable, risking large-scale economic collapse, and even jeopardizing U.S. national security by leaving many Americans victims of a cruel, unjust profit-centered system.

Comparing public health spending with national defense spending further outlines the misinformed decision-making practices of U.S. leaders. The United States spends more than $2,000 per capita on its military budget and a significant amount on the president's security detail. In fact, the proposed budget for the U.S. Secret Service—a federal agency responsible for the protection of the President, Vice President, Presidential Candidates, former Presidents, and their families, along with other political leaders and foreign dignitaries—is $2.4 billion for the fiscal year 2021. This alone is roughly a quarter of the Centers for Disease Control and Prevention's (CDC) average budget—an agency tasked with the protection of 330 million Americans.
Contrasting the CDC's functional budget of approximately $10 billion with the Defense's budget of $740 billion, exposes misaligned national security priorities. Despite this enormous defense spending, the President's life was put at risk, threatening U.S. national security and stability, which could have been avoided with fully funded public health systems and universal health-care coverage ensuring a timely response and containment of the pandemic. Unfortunately, public health spending has continued to decrease, while both military and the current inefficient and expensive health-care system spending has continued to increase, guided by an ill-informed, and otherwise rare, bipartisan consensus. The proactive solution is to invest in public health and universal health care to close the coverage gaps and reduce national security risks.
Comparison of Public Investment in the CDC and the Pentagon
2020 approriations, in billions of dollars, shown for the federal agency and the U.S. department
Underfunded Public Health: National Security Threat to U.S. Armed Forces
Despite limited research efforts to examine the intersection of public health and national security, there is still a precedent for declaring certain infectious diseases risks to national security. For instance, HIV/AIDS was declared a national security threat by the U.S. Government in 2000). The U.S. National Intelligence Council has argued that infectious diseases are a threat to U.S. national security, stating in a National Intelligence Council report, that infectious diseases will "endanger U.S. citizens at home and abroad, threaten U.S. armed forces deployed overseas, and exacerbate social and political instability in key countries and regions in which the United States has significant interests." Public health emergency preparedness has been understood by the public health experts as "the capability of the public health and health-care systems, communities, and individuals, to prevent, protect against, quickly respond to, and recover from health emergencies, particularly those whose scale, timing, or unpredictability threatens to overwhelm routine capabilities." It is clear from the federal response to COVID-19 that public health emergency preparedness, a critical aspect of protecting our nation's security, is not a priority for political decision-makers.
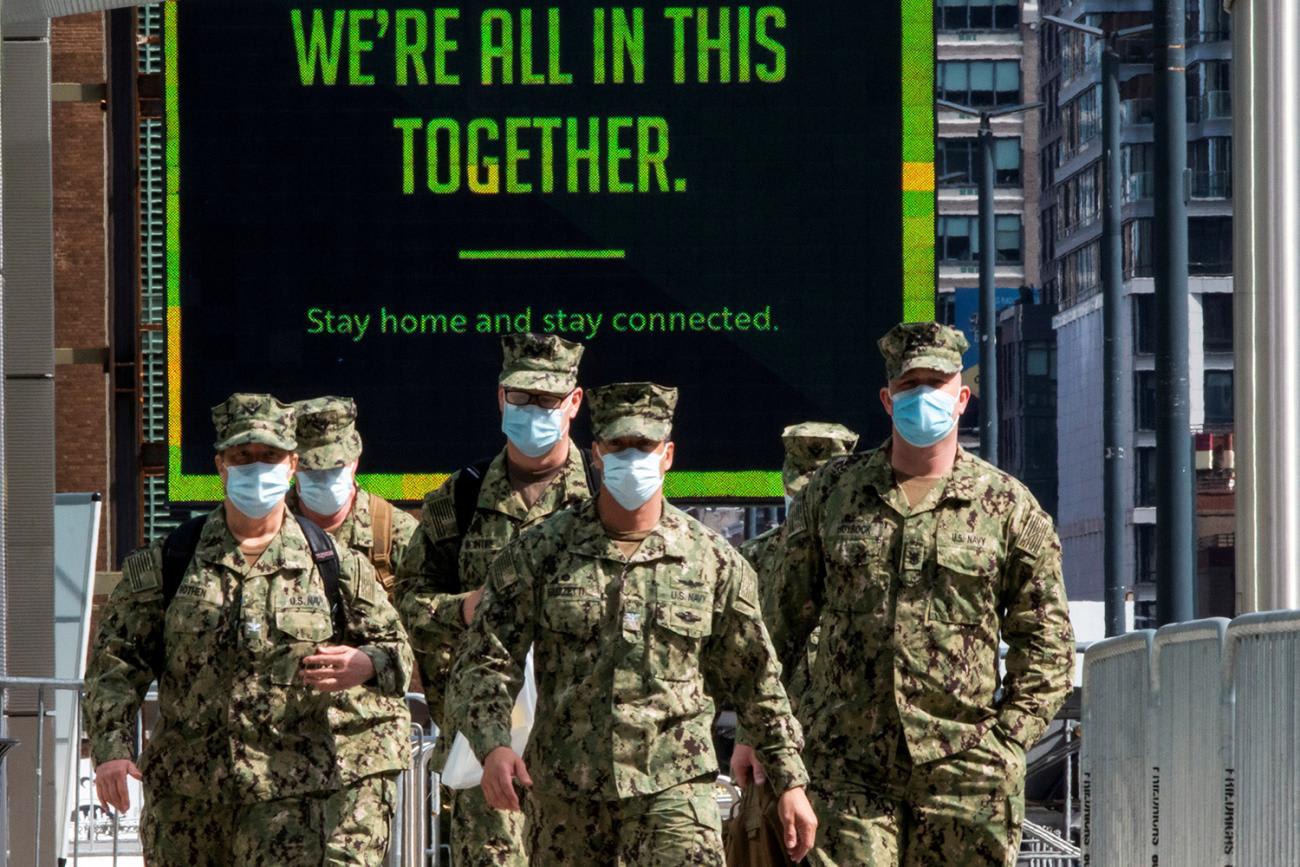
Public health emergency preparedness is not a priority for political decision-makers
While the general health of U.S. citizens remains an acknowledged concern of national security, COVID-19 presents an immediate risk to our military personnel, potentially limiting eligible recruits and adversely impacting military readiness. Inadequate preparation and delayed implementation, as reflected in the current response to COVID-19, places substantial strains on our public health programming, our armed forces, and our frontline workforce. Chronic hemorrhaging of public health financing has necessitated the use of military personnel and equipment, resulting in widespread illnesses and a tremendous number of preventable deaths. Although military personnel are generally younger and healthier than the general population, the virus does not discriminate by service status or by age. Moreover, healthy people are not immune to COVID-19, and can still develop serious complications, require hospitalization, or even die.
Tragic Ironies and the Pandemic Team…What Pandemic Team?
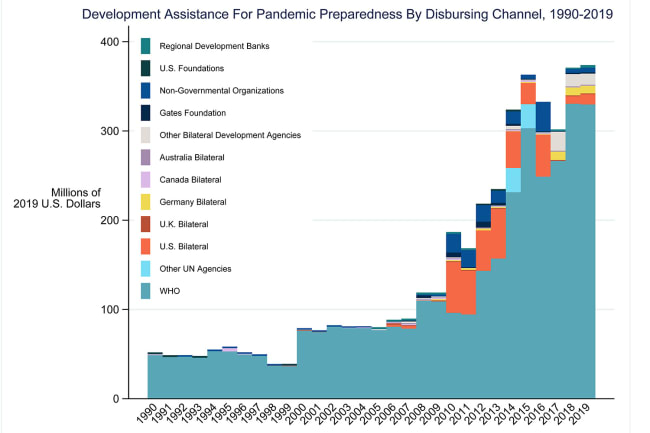
The United States has less than 5 percent of the world's total population, yet represents nearly 25 percent of global COVID-19 cases. On top of consistently scant funding for public health over the years—a trend predating the current administration and transcending political ideologies—this also reflects the current administration's aggressive pursuit of public health defunding and other deregulatory agendas. These initiatives include disbanding the National Security Council Unit, which focused on pandemic preparedness, slashing funds for the CDC, and initially halting funding and eventually withdrawing from the World Health Organization amidst the pandemic. The Tax Cuts and Jobs Act's reallocation of funds from the Prevention and Public Health Fund [$750 million immediately and $1.35 billion over the course of a decade], further burdens public health expansion, especially outbreak responses and immunization efforts. These defunding trends are not unique to the current administration. Defunding public health is a bipartisan practice with policymakers across the political spectrum regularly rolling back public health spending.
Defunding public health is a bipartisan practice with policymakers across the political spectrum regularly rolling back public health spending
In 2018, one study recounted that during the 2009 H1N1 pandemic, only 40 percent of those feeling ill sought medical care within three days. This is concerning considering the role timely access to care plays in reducing mortality, morbidity, and the spread of infection. Without much effort, one can imagine that the 28 million uninsured people, as well as an additional 29 percent who are underinsured, would avoid seeking medical care due to high-cost deductibles and copayments, ultimately contributing to household debt, foreclosure and bankruptcies. A universal health-care system is best equipped to address future pandemics and threats to national security. During pandemics, medication and dispensing supplies costs may vary, which limits access to such critical care. Christina Ho, a professor of law and health policy expert, describes disaster relief Medicaid, which is the precedent for expanding health-care access in the midst of a crisis. Medicaid expansion efforts with low administrative burdens have been implemented in response to natural disasters, the H1N1 pandemic, and lead contamination. Ho further argues the current Administration's inadequate response to COVID-19 and the push for block-grant Medicaid at this time undermines this precise feature of Medicaid, which she describes as, "the open-ended financing structure, that enables it to respond so quickly to unexpected health threats."

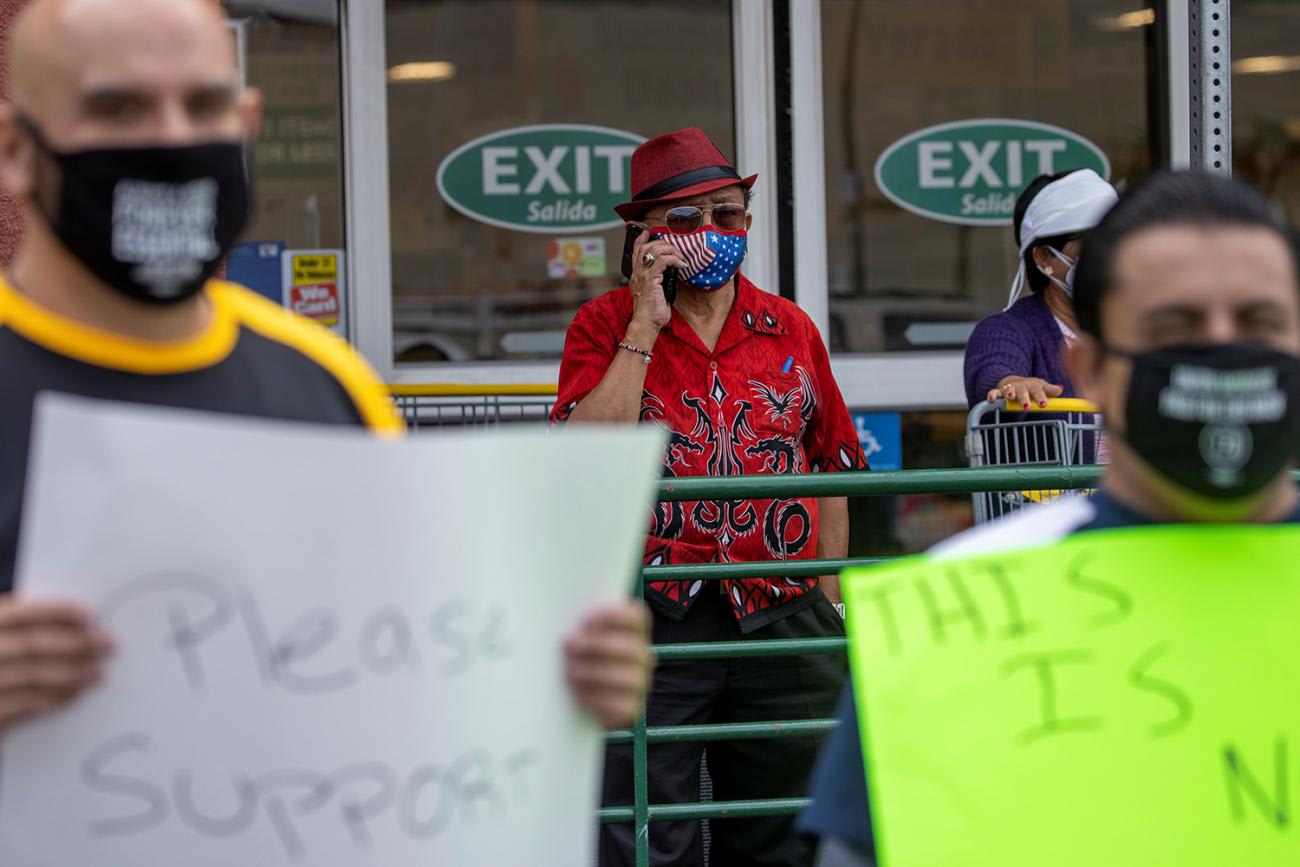
The historical roots of public health are inherently connected with politics and the political economy. Ultimately, the public health community should ardently support policies that protect public health. Complicities and inaction maintain the status quo, and the status quo is killing us. Our existing health-care system is conceptually designed to deliver the best health care that money can buy—but only to those with the money. The vast majority of the U.S. population, including the many essential workers who form the backbone of the economy—such as farm and agricultural workers, grocery store employees, health-care workers, and mail delivery service personnel—do not have adequate, if any, health coverage.
Nearly 80 percent of U.S. workers live paycheck to paycheck
COVID-19 made apparent the health gaps between the affluent and privileged and those most marginalized and destitute because of structural issues such as racism. The working poor, functioning as an essential backbone to the economy, is constituted with people from diverse socioeconomic backgrounds, such as race, gender, age, and citizenship status—the majority of whom live paycheck to paycheck (nearly 80 percent of U.S. workers live paycheck to paycheck). Realities of this pandemic reveal the inadequacies and risks of employer-conditioned health care. The current health-care system, including employer-based health insurance, is costly and inefficient. It burdens many with medical debt and denies a significant number of Americans access to quality health care. Yet, many in the public health community fail to acknowledge the undeniable intersection of public health and poor policy. It is time to move past that. We must always rely on the evidence and stay nonpartisan, but we no longer afford to pretend these problems don't exist.
Politicization of Evidenced-Based Public Health Practice
The politicization of evidence-based health-care systems, public health financing, and interventions is nothing new in the United States—even though empirical research should caution policymakers of the drawbacks of politicizing non-partisan health priorities, such as H1N1 influenza or COVID-19. Policies that undermine our nation's public health or exacerbate social inequities put everyone at risk. For instance, states that did not expand Medicaid now face higher rates of uninsured and underinsured people and frequent hospital closings, which reduce access to care and skilled employment opportunities. A total of 47 hospitals closed in 2019 alone, according to the Medicare Payment Advisory Commission. Rural hospital closures reached their highest peak this decade in 2019, and urban regions have also witnessed a dearth of hospitals, skilled health-care workforces, and prescription drugs.
Inadequate public health preparedness increases the vulnerabilities of our nation's health-care system and exacerbates health inequities
In public health crises like COVID-19, health-care access and quality are critical components to achieving the triple aim of public health: improving the experience of care, improving the health of populations, and reducing per capita costs of health care. Inadequate public health preparedness, including substandard funding and infrastructure, increases the vulnerabilities of our nation's health-care system and exacerbates health inequities indiscriminately. Creating sustainable public health funding measures and adopting a universal health-care model may not only strengthen our nation's health security but also help redistribute costs and prevent economic instability. Contemporary research, including the findings of the prominent libertarian think tank, the Koch Family Foundation funded Mercatus Center, supports the fiscal viability of universal health care, with considerable savings associated with plan features and implementation strategies.
Current trillion-dollar COVID-19 response efforts, coalescing with the primacy of health-care industry profiteering, highlight preventable structural factors associated with chronic cuts to public health budgets. Benjamin Franklin suggested, "an ounce of prevention is worth a pound of cure." This sentiment remains true in 2020. The Constitution prominently features economic and social rights but addresses them with little specificity. The preamble states that an overriding purpose of the U.S. Constitution is to "promote the general welfare" of the citizenry, indicating that issues such as poverty, housing, food security, and other economic and social welfare issues were of central concern to the framers. Chronically underfunded public health systems have yet to serve us well. Sustainable, long-term funding for public health planning, which intentionally addresses multifactorial social determinants of health, such as housing security, a livable wage, neighborhood safety, and high-quality education, is non-negotiable for a healthy and resilient society. A properly-funded and universal health-care system is an evidence-based investment in the future of this nation. This will strengthen our national security capacity by reducing the risk of a system collapse.
COVID-19: Snapshot of Future Threats
Unfortunately, the current pandemic will not likely be the last. Continued ecosystem degradation and climate change facilitate the spread of infectious diseases. Further, a U.S. Global Change Research Program workshop report highlights the need for a comprehensive framework, with public health at its principle core, to prepare for and respond to threats at the junction of climate change, infectious disease, and national security.
A properly-funded and universal health-care system is an evidence-based investment in the future of this nation
With climate change leading to changes in weather patterns, rising temperatures and sea levels, thawing permafrost, and progressive food insecurity, infectious diseases will continue to compromise human health. The human health chapter of the recent National Climate Assessment estimates that under a high emissions scenario, similar to the emissions pathway before the implementation of COVID-19 public health response policies, the health-related costs of West Nile neuroinvasive disease alone are projected to be approximately $1 billion per year by 2050 and an additional $3.3 billion annually by the end of this century (in 2015 dollars). Neglecting to prioritize the protection of public health services challenges not only our nation's current state, but it also exacerbates the impacts of climate change and climate-sensitive infectious diseases in the future.

U.S. national security risks can be reduced with well-funded, equitable public health, and universal health-care systems. This will relieve our society of expensive, reactive public policies that may be inadequate, inefficient, or unjust. Moreover, approximately two-thirds of the U.S. public supports some form of a federally funded health-care system conducive to universal coverage. Decades of public health defunding, deregulation, privatization, mistrust of empirical evidence, politicization, and the proliferation of misinformation have led to our current anxiety-fueled state of affairs. Moreover, if recent stock market crashes and boundless job losses are any indications, a universal health-care system is imperative to ensure economic resilience, equitable mental and physical health outcomes, and an international competitive edge.
What does national security mean if we are not protecting our citizens from harm?
Universal health care is a humane, patriotic duty, which is especially crucial for national security, guaranteeing everything from the health of our neighbors to the health of our soldiers. The public health community should galvanize efforts to frame and advocate for these systems through a national security context as well to ensure a much broader consensus as both public health infrastructure and universal health care are social justice issues. We should redefine our social contract and demand a paradigm shift from a primitive medicalized model that prioritizes acute health care above public health. It is time to relinquish bipartisan special interest bidding in favor of supporting evidence-based public health-systems financing and universal health care to achieve a culture of health. After all, what does national security mean if we are not protecting our citizens from harm?