The COVID-19 pandemic has forced focus on health-systems and their capacity to handle strain. News headlines have been dominated by shortages of personal protective equipment, inadequate testing supplies, municipal hospital beds reaching capacity, and emergency construction of makeshift structures to contain patient overflow. The capacity and robustness of health-systems around the world have been laid bare during this global pandemic—just when they have never been more critical.
Funding for health-systems strengthening was 14 percent of total development assistance for health—$5.6 billion—in 2019
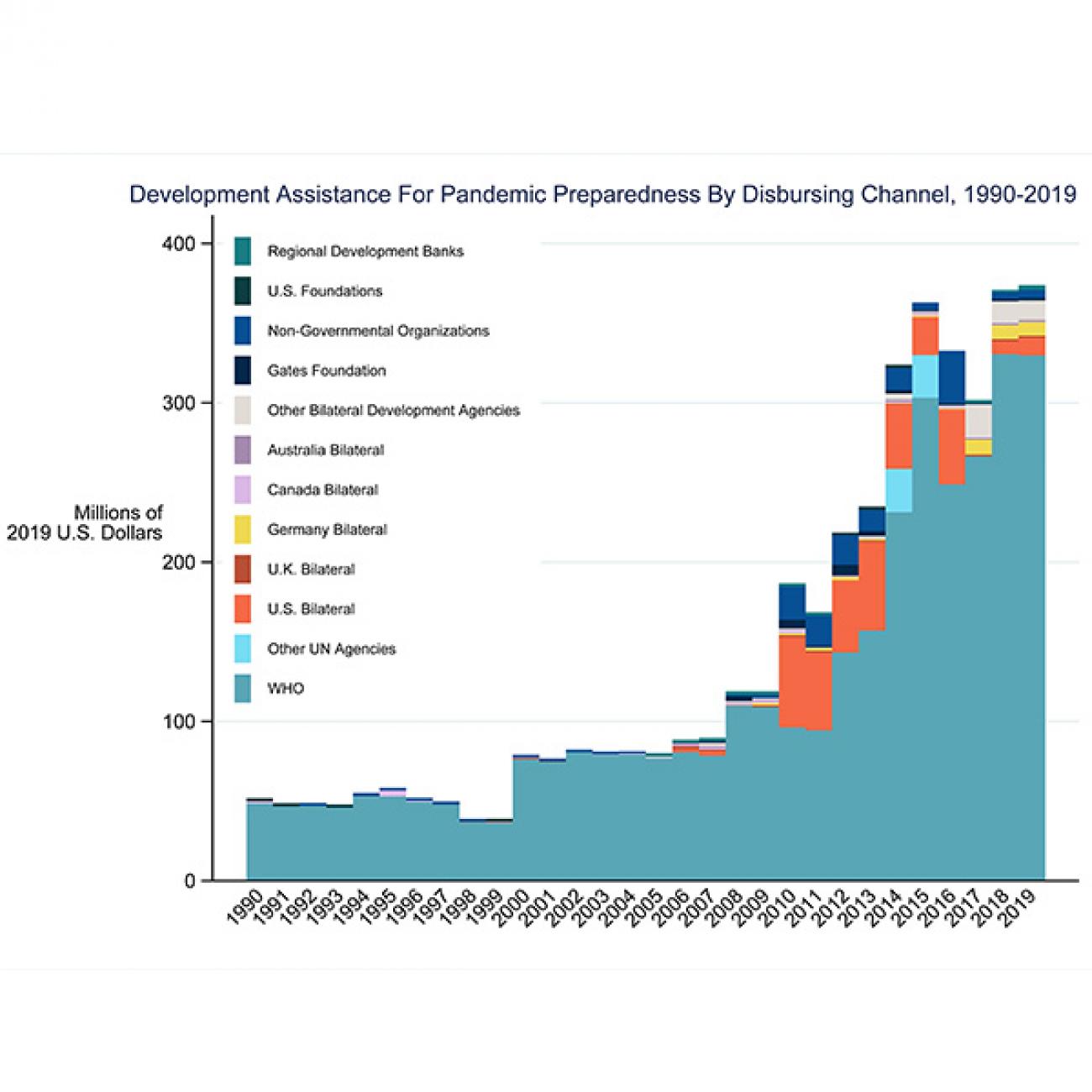
Over time only a smaller share of development assistance for health has gone towards health-systems strengthening activities. These contributions have gone to support activities such as health worker training and updating cold chain equipment systems, which are essential inputs for health-systems to run smoothly. Funding for health-systems strengthening has also been aimed at instituting policies that streamline or enhance the process of procuring medicine and medical supplies. According to the Institute for Health Metrics and Evaluation (IHME) latest financing global health report, Tracking Health Spending in a Time of Crisis, which two of us co-authored, even though total funding for health-systems strengthening has increased over time, it has shrunk as a percentage of total development assistance for health, down from 21 percent ($1.6 billion) in 1990 to 14 percent ($5.6 billion) in 2019.
Why Does Funding for Health System Strengthening Matter?
As the pandemic has unfolded, one fact has become increasingly clear: having a robust health system is the result of complex inputs and processes that may not be taken for granted. How these inputs and processes are undertaken is country- and context-specific. And while these actions are determined by each country for themselves, an increasingly globalized world has heightened the likelihood that an outbreak in one corner of the world can soon become a global pandemic if prompt containment measures are not implemented. Furthermore, strong health-systems can be even more essential when outbreaks spread. As such, contributions that strengthen health-systems in low- and middle-income countries may reduce the likelihood of a global pandemic and enhance global health security for all.
Strong health-systems can be even more essential when outbreaks spread
The World Health Organization (WHO) defines health-systems strengthening as “the process of identifying and implementing the changes in policy and practice in a country’s health system, so that the country can respond better to its health and health system challenges.” The WHO’s health-systems framework outlines six key indicators that make for strong health-systems, including service delivery, governance, health workforce, information, medicines, and financing. According to the WHO, the strength of a health system is measured by an array of factors, ranging from access to affordable care to health worker training.
How Can Funding for Health System Strengthening Be Improved?
Advocates such as The World Health Organization, the World Bank, and the Danish International Development Assistance have promoted sector-wide approaches, which direct donor funding to a pooled fund from which only activities in the national health sector plan are supported, as an approach that increased a country’s ability to direct the use of health system strengthening funds.
Better ensuring that any future outbreaks are contained and do not spread easily
Our analysis shows that much of the development assistance for health-systems strengthening is still focused on specific diseases, which lessens country ownership in the use of funds by restricting their use. It is possible that any type of strengthening funding may ultimately be useful in a health-system. However, when countries are able to direct resources to strengthen the weakest aspects of their health-systems, they are far more able to prioritize and address the most critical local health-systems' needs. Rallying support for health-systems strengthening is more important than ever. While it may seem like a daunting task given the economic downturn caused by the COVID-19 pandemic, focusing the limited resources available for interventions to bolster broader health-systems will be good for global health security by better ensuring that any future outbreaks are contained and do not spread easily.

EDITOR'S NOTE: The authors are employed by the University of Washington's Institute for Health Metrics and Evaluation (IHME), which produced the development assistance for health research described in this article. IHME is a partner on Think Global Health. All statements and views expressed in this article are solely those of the individual author and are not necessarily shared by their institution.