On May 12, a headline in Foreign Affairs declared "Sweden's coronavirus strategy will soon be the world's." What would it look like if the world embraced Sweden's strategy? Most likely, many more deaths from COVID-19. While many of its European neighbors enacted strict lockdowns, Sweden took a very different approach to COVID-19. Its approach, which enjoys widespread support among Swedes, is based on "nudging" people, not forcing them, to comply with social distancing guidelines. The government aims to slow the spread of the virus so that the health system can provide high-quality care to those who fall ill but not shut down the economy. But this approach appears to be costing it dearly in terms of lives lost to the coronavirus.
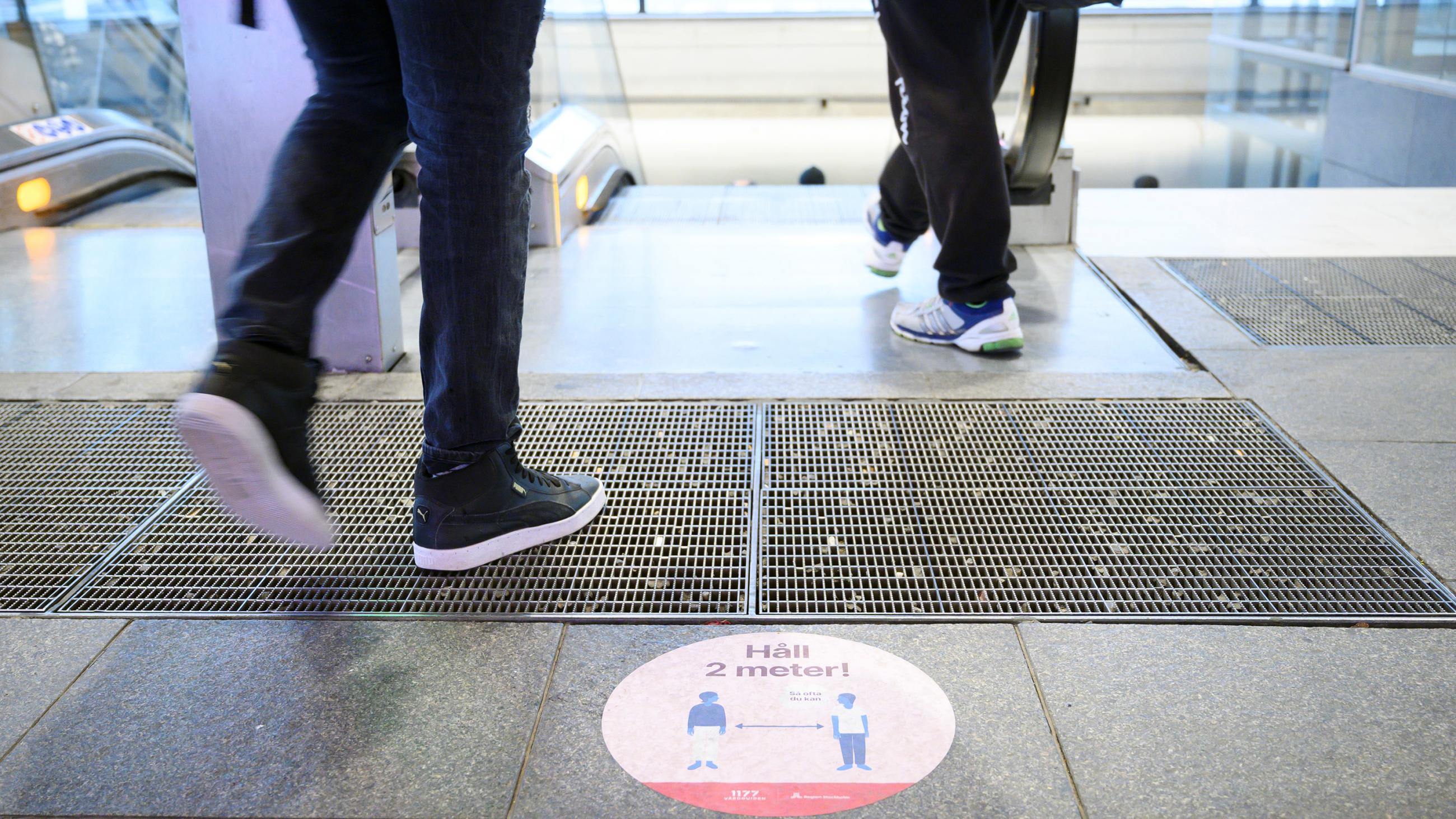
'Nudging' people to comply with social distancing guidelines
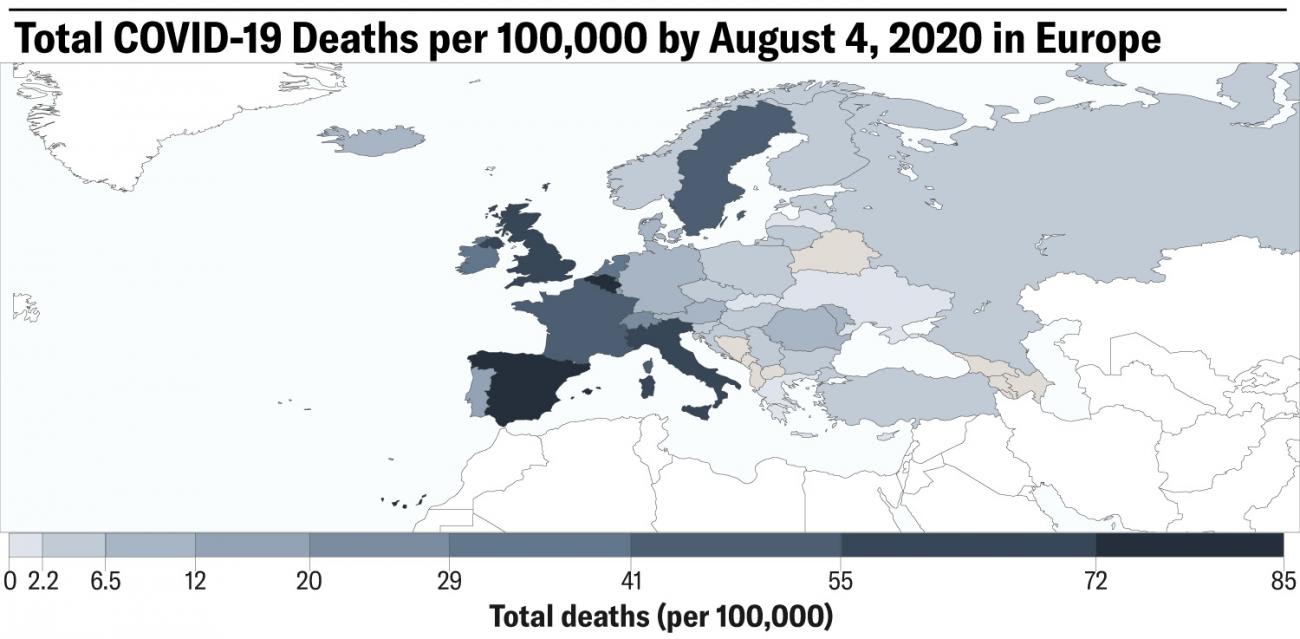
While Sweden has managed to avoid a surge of COVID-19 patients overwhelming hospitals to the same degree seen in the UK, Italy, and New York, the country has been hit much harder by COVID-19 than neighboring Norway, Denmark, and Finland according to University of Washington's Institute for Health Metrics and Evaluation (IHME) forecasts. As of May 29, IHME projects that Sweden's number of total deaths per 100,000 people by August 4 will be on par with France.
Why does Sweden have such poor COVID-19 outcomes relative to its neighbors? Let's examine some of the factors that are working against Sweden.
Problem #1: Voluntary Social Distancing Measures Haven't Reduced Movement Enough
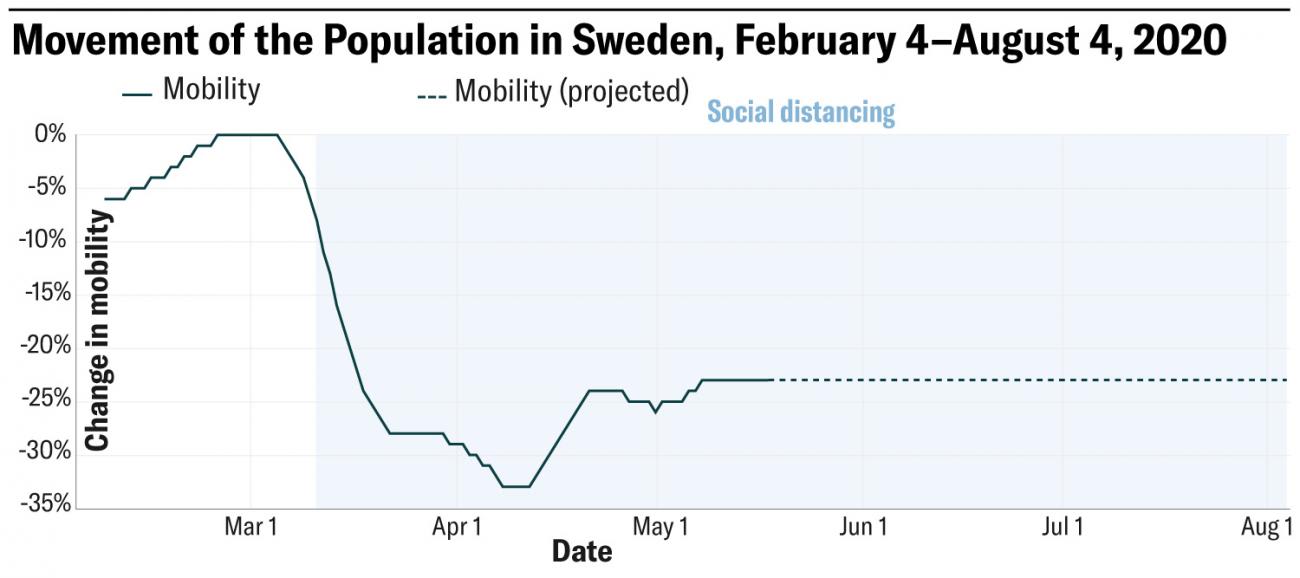
The lower the movement, the lower disease transmission. Even though Swedes decreased their movement in response to the government's voluntary social distancing guidelines, their mobility did not drop as steeply as it did in other places. In Norway and Denmark, for example, mobility dropped by 59 percent and 60 percent, respectively, at its lowest point, while Sweden's mobility dropped by a maximum of 33 percent (Figure 2).
Problem #2: Sweden is far From Reaching Herd Immunity
Although herd immunity has never been an official goal of the government's effort to combat COVID-19, Swedish officials had said it was likely that Stockholm would reach herd immunity sometime in mid-May.
Only 7 percent of Stockholm's population had developed antibodies to the virus by late April—far from herd immunity
Reaching herd immunity, where around two-thirds of the population has antibodies to coronavirus, could potentially help protect the city's population from a second coronavirus pandemic. This seems unlikely to occur any time soon, however. A new study revealed that only 7 percent of Stockholm's population had developed antibodies to the virus by late April. By comparison, even in hard-hit New York City, the percentage of the population with antibodies was found to be 20 percent. Stockholm's level of immunity seems more comparable to the city of Miami, where a random sample of the population revealed that antibodies were present in around 6 percent of the population. While many have touted herd immunity as a benefit of the Swedish strategy, the payoff is far from certain. In Sweden's case, the cost seems to be thousands of preventable deaths.
Problem #3: Elderly People Have Borne the Brunt of the Crisis
Around 90 percent of COVID-19 deaths have occurred in people over seventy years old. Coronavirus has ravaged a vulnerable population that could not follow the government's advice to avoid contact with others—people in nursing homes. In response to these concerns, Swedish prosecutors launched a preliminary investigation into a nursing home in Stockholm with a large number of deaths on May 8.
Problem #4: Disease Transmission Remains High Compared to Neighboring Countries
Low levels of infection give public health measures (testing, isolation, and contact tracing) the best chance of succeeding to contain the virus. The number of infections continues to be substantially higher in Sweden compared to other Nordic countries. Infections in Sweden were estimated at 19.35 per 100,000 on June 2, compared to 1.64 in Denmark, 0.11 in Finland, and 0.24 in Norway. Denmark, Finland, and Norway have been able to get transmission down to a low level largely due to their sharp reductions in mobility.
Problem #5: Testing in Sweden has Lagged Behind
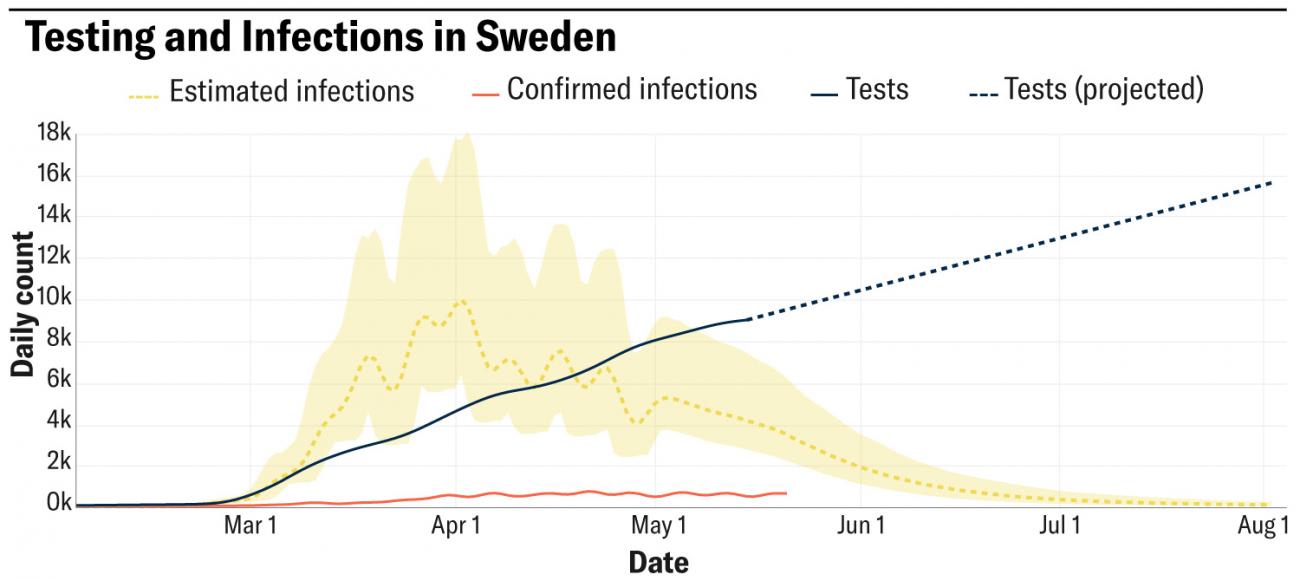
To prevent the virus from spreading undetected through the population, it is vital to have sufficient testing, and the isolation and contact tracing associated with it. Testing needs to keep pace with, and ideally be well above, infections. Having this buffer is important in case there is a sudden resurgence in infections. IHME estimates that Sweden's testing was five times higher than estimated infections as of June 2.
Testing needs to keep pace with, and ideally be well above, infections.
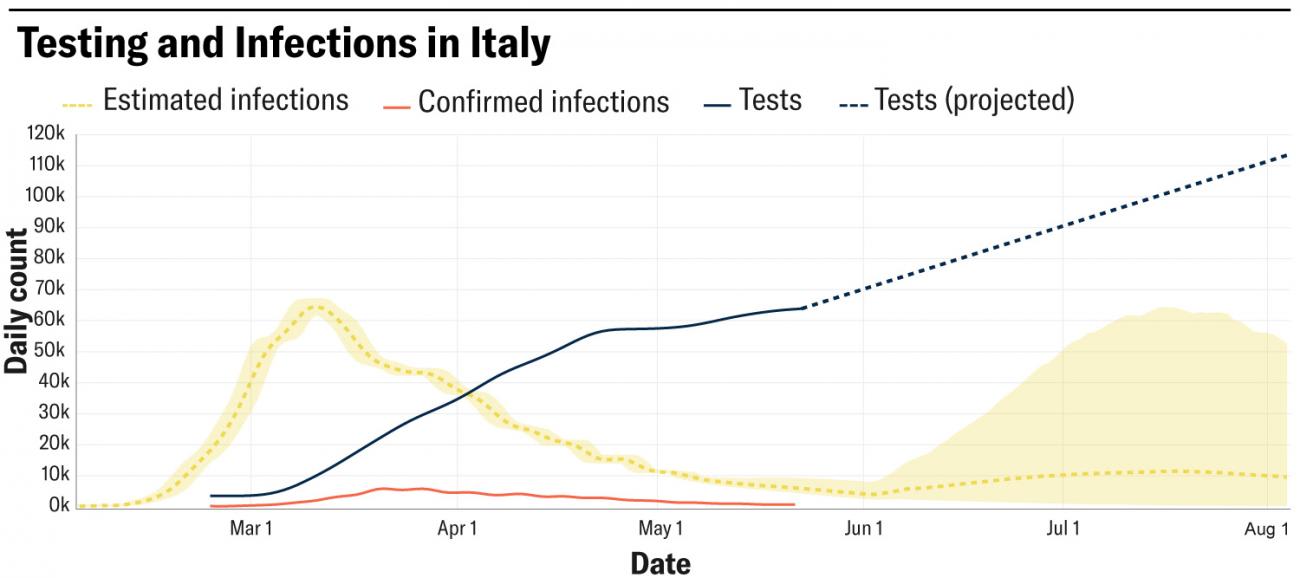
Sweden's buffer between testing and infections is lower than levels seen in other Nordic countries. Should infections start to surge again in Sweden, they could quickly surpass testing levels, and overwhelm Sweden's ability to isolate cases and trace their contacts. For comparison, in countries such as Norway and Denmark, testing levels are well above infections. IHME estimates that testing is 280 times higher than infections in Norway, and 110 times higher than infections in Denmark. Italy's testing levels are also substantially higher than estimated infections, with testing levels nearly eighteen times higher than infections.
Despite these grim trends, recent data coming out of Sweden has shown encouraging signs: COVID-19 deaths are declining, and the most dire predictions appear unlikely to pan out.
Recent data coming out of Sweden has shown encouraging signs
IHME's projections for total deaths in Sweden have declined substantially over time, mainly due to new data on daily COVID-19 deaths showing a drop. Between May 4 and May 29, IHME's projections for total COVID-19 deaths in Sweden were cut in half, and are projected to reach 5,258 by August 4. Also, Sweden seems to have so far escaped the fate of the large COVID-19 death tolls seen in New York and in the United Kingdom despite its relatively relaxed approach to combatting coronavirus.
What has worked in Sweden's favor?

- Lower population density compared to other places hit hard by COVID-19. Higher population density is associated with greater disease transmission. Compared to locations such as New York and the United Kingdom, Swedes don't live as close together. Sweden's population density is comparable to its Nordic neighbor Denmark. The outbreak in Sweden has been concentrated in places where people tend to live close together, such as nursing homes and some low-income neighborhoods.
- Sweden has issued strong guidelines on social distancing. The Folkhälsomyndigheten (Public Health Authority) has recommended that Swedes avoid non-essential travel for greater than two hours by car, and stay at home as much as possible. It has also advised everyone over the age of seventy to avoid contact with others.

- Many Swedes appear to be following social distancing guidelines. In response to social distancing guidelines, movement (mobility) in Sweden started declining in early March, dropping 33 percent by April 8. Since then, mobility has increased by around 10 percentage points. Less contact may translate to lower transmission of disease, so the reduction in movement that began in March may have helped contain the spread of the virus.
- Sweden detected the virus early, putting people on alert. Sweden began testing at the beginning of its COVID-19 epidemic, which enabled the government to warn people about the virus. Compared to Italy, where the virus began spreading exponentially before the first cases were detected, Sweden's head start on testing helped it monitor transmission. Italy had the first coronavirus outbreak in Europe, which alerted other countries on the continent to be on the lookout for the virus.
Despite some signs of progress, Sweden's experience appears to be a cautionary tale. Its death toll far exceeds its neighbors, and its economy is faltering even though it imposed fewer restrictions on movement.
So far, the coronavirus strategies worth emulating seem to lie across Sweden's border
In contrast, the social distancing measures imposed by the governments of Norway, Denmark, and Finland have dramatically reduced deaths and infections in those countries, boosting their chances of containing the virus as they reopen. But in Sweden, challenges in controlling the spread of coronavirus may cause visitors from neighboring countries and elsewhere to stay away, potentially inflicting economic pain for months to come. Concerns about cross-border disease transmission are proving to be a source of political tension in the region. Both Norway and Denmark have opened their borders to each other, but they remain closed to Swedes.
The pandemic is far from over, and IHME will continue updating its projections to understand how COVID-19 trends are evolving in Sweden. So far, the coronavirus strategies worth emulating seem to lie across Sweden's border.
EDITOR'S NOTE: The authors are employed by the University of Washington's Institute for Health Metrics and Evaluation (IHME), which produced the COVID-19 forecasts described in this article. IHME collaborates with the Council on Foreign Relations on Think Global Health. All statements and views expressed in this article are solely those of the individual authors and are not necessarily shared by their institution.












