In recent weeks, we are learning about more and more people in our networks—both personal and professional—who have sought out a supplementary COVID-19 vaccine shot against the guidance of U.S. health officials. And by and large, they are affluent white people.
There is no public data available to tell us who in the United States is getting "booster" shots, but we suspect that the trends mirror what we saw in the initial vaccine rollout, with privileged individuals accessing vaccines much more easily than people with lower incomes. With solid data pointing to the need for COVID-19 vaccine boosters, the U.S. government needs to put the groups who can benefit most from these boosters at the front of the line.
The U.S. government should begin rolling out COVID-19 booster shots for people who are immunocompromised, adults aged 60 and older, racial and ethnic minority groups, health care workers and other essential workers, people experiencing homelessness, and incarcerated people. The longer we wait to provide booster shots to those who need them most, the greater the risk of outbreaks in places where we can least afford them.
The U.S. government needs to put groups who can benefit most from booster shots at the front of the line
Our health-care workers, many of whom received their first dose in December 2020 and January 2021, could transmit COVID-19 to patients amid the current Delta variant surge. The Israeli government's research shows that the Pfizer vaccine's ability to prevent infection dropped to just 16 percent among those who were vaccinated in January 2021, yet it remains highly effective at preventing people from being hospitalized or dying. While it's great news that the vaccines are still working to save lives, even against Delta, no one wants their immunocompromised loved one to get COVID-19 from a health-care worker at, for example, their chemotherapy appointment. While personal protective equipment such as masks can substantially lower transmission of COVID-19, we need to employ every useful tool we have against the highly transmissible Delta variant.

Early data indicates that boosters are a vital tool to control COVID-19—Pfizer found that a third vaccine dose increases a person's virus-fighting antibodies up to one hundred times higher than pre-vaccination levels. Booster doses can improve immunity and reduce the spread of COVID-19, so we need to start deploying them quickly as upticks in so-called breakthrough infections mount. Breakthrough infections are occurring even in places where vaccination rates are high. For example, even in Iceland, where currently 75 percent of people are fully vaccinated, variant-linked cases are increasing. And in the United States, three quarters of the people who were recently infected in a COVID-19 outbreak in Massachusetts were fully vaccinated. Breakthrough infections not only threaten our health, but can also undermine trust in vaccines. We need to bolster immunity and vaccine confidence with booster shots.
People who are at higher risk of dying from COVID-19, including older adults and immunocompromised individuals, should get booster shots right away. The data from Israel indicates that breakthrough infections are happening among vaccinated people of all ages—older adults do not appear to have a greater risk of a breakthrough infection than a younger person. So older adults and immunocompromised people should receive access to boosters at the same time.
Early data indicates boosters are a vital tool to control COVID-19—Pfizer found that a third dose increases a person's virus-fighting antibodies
Teachers, school staff, and childcare workers are another group who will need booster shots to protect unvaccinated children. Many school staff and childcare workers received their vaccines in March. With schools reopening in August and September across the United States, and large groups of unvaccinated children attending school in person, the likelihood that fully vaccinated adults could pass infections to unvaccinated kids will increase as Delta rips through communities. Schools and childcare centers will be filled with vulnerable kids—including children under 12, who are not yet approved for vaccination. And currently, less than a third of children 12 to 15 are fully vaccinated.
Prioritizing school employees and childcare workers for boosters is even more urgent because many received priority access to the Johnson & Johnson vaccine across numerous states amid the push to reopen schools quickly last spring. The Johnson & Johnson vaccine is less effective than the Pfizer and Moderna vaccines at preventing infection, so it is likely that people who received this vaccine will have even lower immunity six months post-vaccination compared to people who were vaccinated with Pfizer or Moderna.
We must double our efforts to break down barriers to COVID-19 vaccination for Black, Latino, and Indigenous Americans
For individuals who are from racial and ethnic minority groups, systemic racism continues to increase the risk of getting infected with and dying from COVID-19 relative to white people. Lack of access to jobs that can be performed remotely, crowded living conditions, and lower rates of health insurance make boosters essential. Adding to this risk is the fact that rates of vaccination among Black and Latino people in the United States remain lower than in white people. In the initial COVID-19 vaccine rollout, the United States erred when it failed to prioritize vaccines for people in racial and ethnic minority communities.
We must get it right with boosters. As Dr. Rhea Boyd noted in a recent interview, "availability and accessibility [to vaccines] are not the same thing." For example, the U.S. government is incentivizing, but not requiring, employers to give employees paid time off to get vaccinated. Without this protection, falling ill from vaccine side effects for one or two days could cost people their livelihoods. As a country, we must double our efforts to break down barriers to COVID-19 vaccination for Black, Latino, and Indigenous Americans, and at the same time prioritize these communities for boosters.

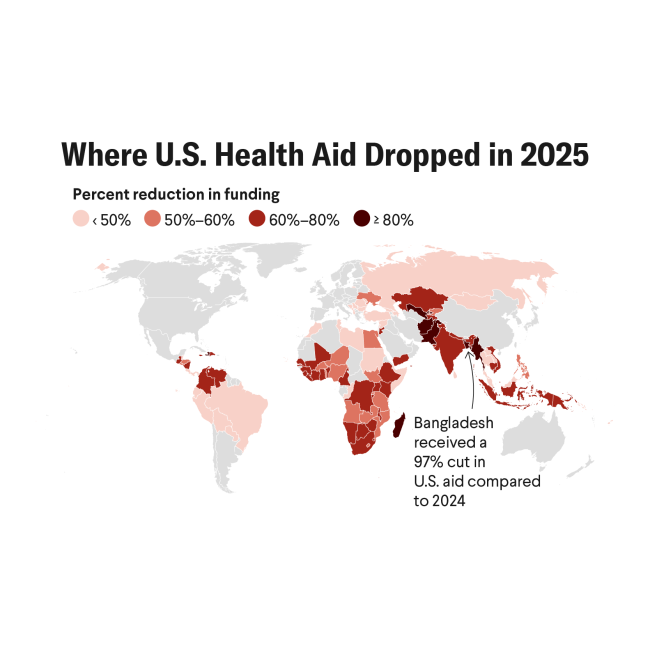
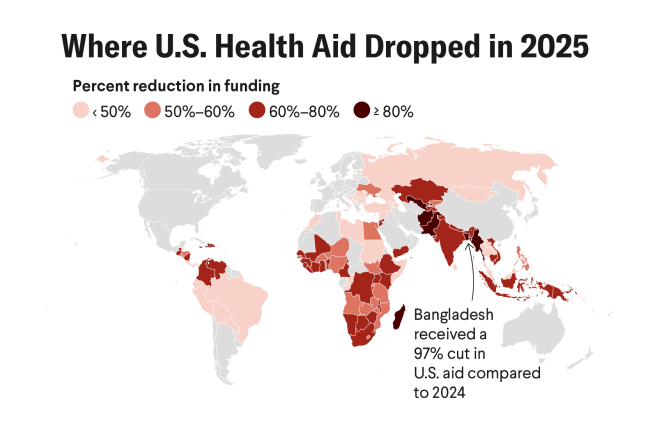
With COVID-19 vaccines and boosters, we can't limit our thinking about equity to our national borders. Currently, just one percent of people in low-income countries have received one dose of a COVID-19 vaccine, and every shot ordered for use in the United States translates to more death and economic devastation in these countries, and it multiplies opportunities for the virus to mutate into even more dangerous forms. Therefore, for the next few months, boosters should be prioritized in the United States only for individuals who are at greatest risk of dying from the disease or have a high risk of spreading COVID-19 infection.
To free up additional vaccines for low- and middle-income countries, the United States should stop throwing away vaccines, instead offering these jabs as boosters to anyone who wants them before they expire. To date, the United States has wasted at least one million doses of COVID-19 vaccines since December. This wastage is unconscionable. Immediately, the government should allow vaccine providers to give these unused doses away before they go to waste. Unfortunately, doses that are about to expire can't be donated to other countries given logistical constraints, but they can be used to reduce the demand for booster doses nationwide so that future vaccine supplies are freed up for donations.
Wealthy countries should develop a global version of "Operation Warp Speed" to help low- and middle-income countries produce mRNA vaccines
But donations alone will not suffice to vaccinate the world. Wealthy countries, including the United States, should develop a global version of "Operation Warp Speed" to help low- and middle-income countries produce mRNA vaccines.
Entering the eighth month of our vaccination campaign here in the United States, some Americans are seeking out unauthorized booster shots. As cases surge in nearly every corner of our country, it's time for the government to make sure that boosters are reaching the people who need them most instead of the people who are cheating the system. The Delta variant will take advantage of every extra day that we give it to spread.

EDITOR'S NOTE: Ali H. Mokdad is employed by the University of Washington's Institute for Health Metrics and Evaluation (IHME), which produced the COVID-19 forecasts described in this article. IHME collaborates with the Council on Foreign Relations on Think Global Health. All statements and views expressed in this article are solely those of the individual authors and are not necessarily shared by their institution.