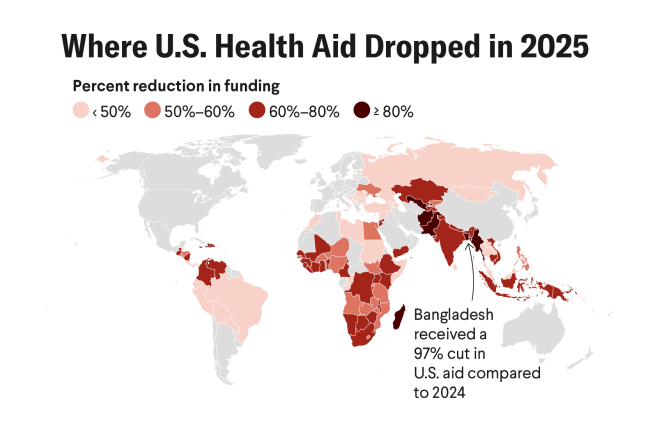
The fallout from dismantling the U.S. Agency for International Development (USAID) presents opportunities to think about global health, development, and sexual and reproductive health differently. The existing health infrastructure is extremely fragile. All it took was a single U.S. election to reveal the imbalance of power and the fragility of current aid approaches.
Countries are struggling to maintain stable delivery of health care for their people. In Ethiopia, contracts of more than 5,000 health system employees have been terminated. In Malawi, observers predict stock shortages for family-planning commodities and drugs for HIV/AIDs and tuberculosis. In Kenya, the funding freeze precipitated job losses for 54,000 health workers. The illusion that the United States was building sustainable health systems was just that, an illusion.
Low- or middle-income countries (LMICs) use external aid to support basic functions, not "nice-to-have" extras such as green spaces. Thus, for many countries, the health and well-being of their citizens hinges on politics in a donor country. The U.S. decision to withhold aid exposed LMICs' dependency on foreign assistance. It also brought to light some governments' unwillingness to meet their obligations as well as nongovernmental organizations' (NGOs) and some donors' desire to keep governments dependent. These new financial constraints are forcing countries, NGOs, and donors to make tough decisions about how to use precious resources.
The lack of U.S. support is a real opportunity to reimagine support for sexual and reproductive health and rights. The Helms Amendment and the Mexico City Policy, also known as the Global Gag Rule, are moot without U.S. funding. Together, these policies have massively harmed millions of women for decades. Now, health systems, donors, and organizations of all sizes do not have to adhere to U.S. policies and can provide safe, legal, and lifesaving abortion care.
Health systems can think about sexual and reproductive health services that don't marginalize essential services
Health systems can think about sexual and reproductive health services that don't marginalize essential services, such as abortion care, and integrate them into broader reproductive health services, including postpartum care, contraceptive counseling, comprehensive sexuality education, and much more.
Although the circumstances that led to this inflection point are troubling, immense possibilities remain to build and support more sustainable health systems.
The decolonizing health movement offers ideas on how to reimagine global health in three main areas—knowledge, funding, and practice—where power is often consolidated.
Knowledge
The end of long-standing research and data collection efforts such as USAID's Demographic and Health Surveys makes it clear that the world was dependent on the United States for fundamental information for health planning. The Africa Centers for Disease Control and Prevention and many universities and research institutions in Australia, Canada, and Europe can help assume the U.S. role. In addition, many institutions based in LMICs honor the contributions of their in-country partners through knowledge exchange, shared funding mechanisms, and capacity strengthening. These institutions and partners also commit to turning research findings into practice [PDF].
This opportunity can also elevate forms of knowledge and evidence that fall outside what is generally considered acceptable to modern scientific discourse. Examples include the lived experience of people [PDF], Indigenous knowledge, community health workers both inside and outside the official health system. Contextual knowledge is valuable in understanding and strengthening local health systems, yet may not be transferable.
Funding
Sustainability should be redefined given previous notions that were woefully inadequate. This means providing diversified funding, increasing domestic financing, and addressing the crippling debt many countries face—all things reiterated in conversations heard during the sixty-ninth Commission on the Status of Women (CSW69). In 2024, African countries spent $164 billion on debt financing. Those countries cannot fund their health systems if their annual budgets are going toward debt financing.

The way funding is deployed should also change. The U.S.-dominated model of global health created silos among disease entities, between international nongovernmental groups and community groups, between for- and nonprofit entities, and between research and practice. The result is higher health-care costs, less knowledge exchange, and inefficient health systems.
Projects are designed to meet the needs and imperatives of the donor agencies that support them—everything from performance indicators to ideologies are represented in aid programs. This often results in duplicated efforts in the aid sector. Projects are subject to donor whims, political winds, and the force of personalities.
Movement-based funding that allows for greater fluidity among NGOs and multilateral organizations, and the development of new partnerships is one alternative to the traditional U.S.-supported system. Governments should be serious about efficiency while marshaling all available resources under a common umbrella. Finally, the global health community needs to be real about breaking the development-industrial complex, where donors, government, and NGOs care most about their own survival and bottom line rather than creating sustainable health systems.
Practice
The discussion among other global health actors continues around fostering movements for social change. The reproductive justice movement includes feminist organizations, civil society groups, and international organizations that work on different issues. A movement approach is not based on deliverables or specific outcomes. It is fluid and based on the idea that bringing people and organizations together for a common cause will result in change. At Ipas, we use the sustainable abortion ecosystem as part of the broader movement for reproductive justice. This approach brings together stakeholders and fosters relationships to protect individuals' rights to bodily autonomy and improve abortion access. The model is rooted in human rights, equity, and local expertise, and focuses on several components, such as individual knowledge and agency; community and political support; financing mechanisms that ensure affordable, equitable access to health care; and a trained and supported health workforce.
Governments should be serious about efficiency while marshaling all available resources under a common umbrella
A movement for equity in public health would be another approach to consider. This idea is not new. From the Declaration at Alma Ata to Universal Health Coverage, the global public community has tried to address the underlying social and economic issues related to health outcomes. The criticisms of these approaches include that they are too broad and idealistic. Yet the alternatives, namely, highly targeted, vertical disease-centered approaches have also not succeeded in building sustainable health systems. Now is the moment to embrace the complexity and promise of the primary health-care movement. It is idealistic; it is visionary; it is about social determinants rather than exclusively biomedical interventions; and it is exactly what is needed.
The end of U.S. foreign aid could be permanent, or the funds could be restored and realigned with the values of the Donald Trump administration. If aid does come back, it will likely be even more transactional and restricted in its approach. Given what is seen in other negotiations taken by the Trump administration—from Ukraine to tariffs—ultimatums are likely to be issued to low- or middle-income government officials and countries that are already providing aid. Now is the time to advocate and stand up for a progressive and locally driven vision for sexual and reproductive health and rights and global health. Now is the time to contend with the many flaws in the traditional approach to aid and global health and address them.
Aid recipients should prioritize sectors that build human capital. As the adage says, "define or be defined."