COVID-19 has changed our world. Globally, the World Health Organization (WHO) reports nearly 600 million confirmed cases of COVID-19 and over six million deaths. The number and complexity of the challenges that policymakers should address to improve public health in the wake of COVID-19 are daunting.
One of the most important problems is the failure of public health communication throughout the pandemic. This failure involved ineffective strategies, inept execution, and the inability to counter disinformation. New approaches and capabilities are needed to ensure that public health communication facilitates effective responses to disease threats and rebuilds the public's trust in government.
Theory and Practice
Over seventy years ago, the WHO constitution recognized communication as a fundamental principle in its preamble: "Informed opinion and active cooperation on the part of the public are of the utmost importance in the improvement of the health of the people." However, implementing this principle effectively during serious disease events has too often encountered difficulties. For example, inadequate communication about the outbreak of severe acute respiratory syndrome (SARS) in Hong Kong in 2003 meant that "panic developed in the community and weakened cooperation and support from the public."
Generally, communication missteps arise for epidemiological, institutional, and political reasons. With many outbreaks, officials initially lack sufficient information about the pathogen, treatment protocols, and policy interventions that will best protect health. Problems also happen when government bodies fail to communicate clearly and authoritatively about health threats. Politics can also undermine communication when officials withhold information or skew data to suit political interests.
Politics can undermine communication when officials withhold information or skew data to suit political interests
The COVID-19 Communication Cacophony
Despite public health efforts to learn lessons from earlier disease events, COVID-19 produced cacophony in communications about the pandemic. The discordant array of mismatched sounds, messages, and images confused, instead of clarified, the threat and thwarted rather than encouraged appropriate actions, especially concerning vaccines.
This dissonance was even more disconcerting because policymakers had long stressed the importance of being prepared for pandemics, including readiness to communicate effectively with the public. For example, in 2019, the WHO identified pandemic influenza and vaccine hesitancy among the top ten global health threats. When COVID-19 emerged, the world was hit by a different pandemic, vaccine hesitancy, and comprehensive communication failures that contributed to the grievous toll COVID-19 inflicted globally.
COVID-19 featured familiar communication challenges arising from a novel pathogen, the lack of institutional preparedness, and government officials playing politics with an outbreak. However, COVID-19 was the first pandemic that unfolded in an information environment transformed by the internet, especially by social media. Informed and well-intentioned efforts to communicate about the threat and appropriate countermeasures (for example, masking and vaccines) were often overwhelmed by dissemination of sensational misinformation and deliberate disinformation. This "infodemic" became a "second pandemic" that harmed how people understood COVID-19 and how they protected themselves from the disease.
Probing this communication cacophony more reveals three interrelated issues that deserve more attention—the loss of trust in government information sources, the use of ineffective communication strategies, and the pernicious impact of organized disinformation.

Loss of Trust
COVID-19 emerged into a world increasingly characterized by the diminution of trust in government institutions. Analysis has shown that, when people facing health threats do not trust the government, their willingness to adopt protective behaviors recommended or mandated by the government diminishes—as happened during the 2009 H1N1 pandemic, the 2014–2016 West African Ebola epidemic, and COVID-19. Research by Thomas Bollyky, Heidi Larson, and others has corroborated the importance of trust in public institutions.
The communication problems experienced during COVID-19 reinforce three foundational elements for effective communication, which roughly follow the fundamentals of Aristotelian rhetoric on persuasion—ethos, pathos, and logos. To begin, public perceptions of a government's credibility and effectiveness in responding to health threats matter. The connection that individuals and communities have with leaders who communicate information is also important, including whether those leaders exhibit health literacy and emotional and cultural sensitivities. Finally, the willingness of citizens to accept and comply with modern, science-based preventive and protective measures against health threats is critical.
Vaccine hesitancy and opposition during COVID-19 reflected problems with each foundational element of effective communication. High vaccination levels are an indicator of a functioning health system, vaccine-literate populations, and effective public health policies. COVID-19 demonstrated that a fundamental tenet of public health—vaccination—is at risk as a credible defense against disease and illness.
The importance of vaccines for controlling COVID-19 challenged governments to develop and implement trusted, credible, and effective communication strategies. The first vaccine approval in the United States triggered hopes that vaccines would change the pandemic's trajectory. However, experts warned that getting people vaccinated required a sustained and trustworthy communication system funded to engage in campaigns linked with community-level efforts.
The difficulties with U.S. vaccination efforts concerning COVID-19 revealed a widespread loss of trust in government institutions, which undermined the credibility and effectiveness of government communications. According to the U.S. Centers for Disease Control and Prevention (CDC), as of August 22, 2022, 67.4 percent of the American population are fully vaccinated, but only 33.2 percent of adults between 50 and 64 years old have received their second booster. A paltry 4.8 percent of children under the age of five have received their first vaccine shot, and less than 1 percent are fully vaccinated and boosted. Less than 25 percent of eligible 5- to 17-year-olds are fully vaccinated and boosted. Shockingly, 21 percent of Americans are not vaccinated at all.
Twenty-one percent of Americans are not vaccinated against COVID-19
Ineffective Strategy
The U.S. communication response to the pandemic lacked a strategic approach to mitigate and manage the risks of COVID-19. Before the WHO called COVID-19 a pandemic, experts identified the need for a coordinated, trusted source of communication. Unfortunately, the opportunity to establish credible and trusted communications to prepare the public to understand COVID-19 and support the vaccination effort was missed.
An effective communication strategy should include collaboration with different types of media to disseminate appropriate messages to targeted audiences. People have varying levels of health literacy, readiness to make health decisions, and ideological orientations. Tailored, dynamic communication campaigns designed to reach such diverse groups needed to engage multisectoral partners with information sources trusted by these communities. This communication imperative also went unmet in the United States.
When recently announcing a reorganization of the CDC, Director Rochelle Walensky acknowledged that the agency is "responsible for some pretty dramatic, pretty public mistakes, from testing to data to communications." Among the planned reforms, Walensky emphasized the need to "deliver clear, concise messages about public health threats."
Organized Disinformation
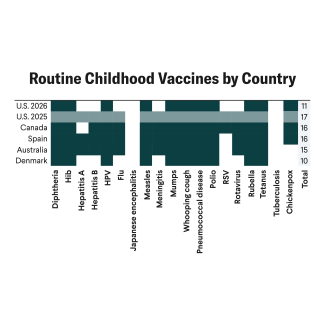
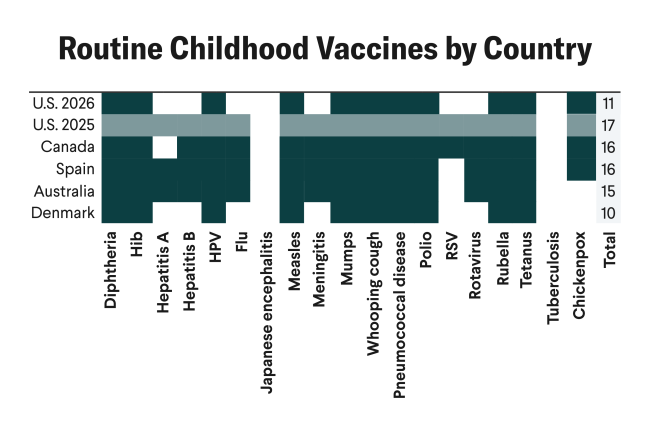
Communication strategies that embrace behavioral economics, health literacy, and communication levers (for example, news and social media) drive citizens toward healthier decisions. By contrast, the online ecosystem facilitated the premediated and reckless spewing of unsubstantiated information that created doubts about COVID-19 and the vaccines developed for it. The anti-vaccination movement had existed before COVID-19, but it strengthened its internet presence and impact during the pandemic and became an antivax tsunami dangerous to vaccinations for diseases beyond COVID-19.
The U.S. Surgeon General's report on Confronting Health Misinformation recommended urgently moving "toward coordinated, at scale investment to tackle misinformation." This proposal underscores the need for a well-resourced strategic plan to overcome the global antivax movement. This plan could include active monitoring of online misinformation and disinformation and the use of artificial intelligence software to identify, track, and disrupt attempts to undermine public health activities, including vaccination. Refuting myths, misconceptions, and malign intentions on vaccination while promoting health literacy through trusted sources and materials are fundamental for success.
INSIGHT for Action
The problems experienced during COVID-19 highlight that the lack of an authoritative and trusted communication strategy and system makes societies vulnerable to disease outbreaks and disinformation designed to undermine effective public health responses. The communication challenges and controversies created by the monkeypox outbreak again reveal this vulnerability.
The United States has never developed an integrated public health communication system as it has done for homeland security threats and weather events. The United States should adopt an Initiative to Strengthen Information on Global Health Threats (INSIGHT) to be the recognized, credible, and trusted source of information. INSIGHT could integrate identification, tracking, and real-time communication for effective responses concerning public health threats.
The Task Ahead
Improving public health communication after COVID-19 faces long odds. Despite the damage done, the emergence of new variants, ongoing streams of new cases and deaths, fatigue, and complacency about COVID-19 are eroding vigilance. The lack of trust in government institutions apparent during the pandemic has not abated, and disinformation about vaccines and disease threats remains dangerous for the public's health.
This difficult context only increases the importance of investing in strategic health communication capabilities that can provide credible and trusted information to support policies that prevent, protect against, and control threats to population health. As the United States finds its way out of the COVID-19 pandemic and prepares for the next one, leaders can and should do better to ensure that informed opinion and active cooperation among the people support the improvement of public health.