Wherever people look, climate change is inflicting ever greater physical, economic, and mental costs on people and communities. From the impact of extreme weather events on food security to the growing spread of infectious diseases as weather patterns change, and with the rise of deadly heat waves, it is undeniable that what harms our planet also harms our health.
To meet the Paris Climate Agreement targets of limiting global temperature rise to under 1.5°C (2.7°F), every sector—including health care—must undergo decarbonization in adapting to this new reality. Health care is one of many sectors fueling the climate crisis, emitting more global carbon dioxide (CO2) emissions than the shipping industry.
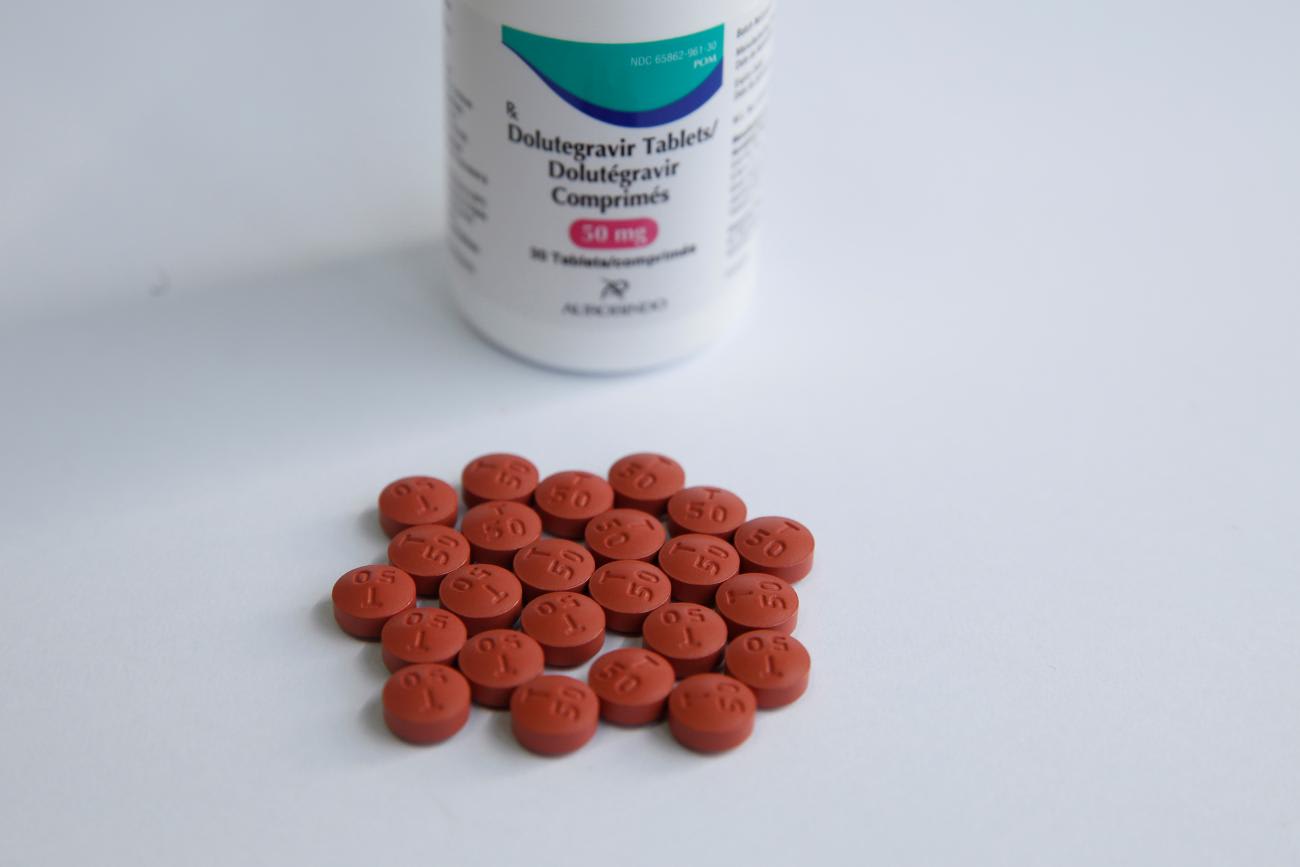
In a new study, Unitaid sought to answer whether switching from one drug to another could provide lifesaving benefits while reducing carbon emissions. The findings reveal that this is not only possible, but also already happening with dolutegravir—the world's leading HIV drug, taken daily by more than 24 million people.
Dolutegravir: A Win-Win for Health and Climate
Dolutegravir-based regimen (referred to as dolutegravir, or DTG) has revolutionized HIV treatment since its introduction. Approved in 2013–2014, it quickly became the standard of care in low- and middle-income countries by 2017, thanks to the efforts of many global health actors, including Unitaid. Relative to its predecessor, efavirenz-based regimen (EFV), DTG provides faster viral suppression, has fewer side effects, and offers greater affordability.
DTG is 2.6 times less carbon intensive than the medicine it replaced
But DTG's impact goes beyond health. Unitaid's latest report reveals that DTG is 2.6 times less carbon intensive than the medicine it replaced. By gradually switching more than 24 million people living with HIV to DTG since 2017, the global health community will prevent 26 million tons of CO2 from entering the atmosphere over the course of a decade. That's equivalent to eliminating the total carbon emissions of Geneva—a city with 206,000 residents—during that same period.
DTG is less carbon intensive for one main reason. It requires only 650 milligrams of active pharmaceutical ingredient (API) per daily dose relative to EFV's 1,200 milligrams. Since API production is the most carbon-intensive aspect of pharmaceutical products, the reduced volume for DTG results in lower emissions.
A Climate Blind Spot
The many global health actors involved in introducing DTG did not do so with the intent to lower carbon emissions but instead purely in pursuit of better public health outcomes. But in doing so, this one single drug unknowingly reduced the health sector's overall carbon footprint in low- and middle-income countries by a whopping 0.3 to 0.4%. This may seem small, but is a magnitude of reduction that surpasses many hard-won climate mitigation achievements in both health and other sectors.
Knowing about DTG's climate value when it was introduced would have been incredibly powerful. As Oyun Sanjaasuren, the Green Climate Fund's director of external affairs, emphasized in the report's foreword, this work highlights a missed opportunity: Had climate considerations been integrated into the rollout of DTG from the start, its carbon footprint could have been reduced even more. This additional argument in favor of DTG could have also accelerated the transition effort, mobilizing more advocates and funders around a clear win-win for health and climate, and unlocking DTG's health, economic, and climate benefits earlier and faster.
These results encourage us to confront the question: Should new medicines or health products be produced with the dual goals of benefiting both patients and the environment? This choice isn't between saving lives or reducing CO2 emissions. Instead, it highlights a gap in health-care policymaking. We need to recognize that climate change directly affects people's health and well-being, especially the most vulnerable. Health and equity are therefore central to both sides of this equation. Although current health-care policies and assessments rarely consider climate and environmental impacts, some promising examples show why understanding both the public health benefit of health products and their environmental impact is important.
Last, the report demonstrates that carbon emissions from health products are not inevitable. Although DTG is less carbon intensive than its predecessor, it still produces significant emissions—as do all health products. Solutions to further reducing this footprint are numerous, from improving process efficiency to better selection of raw materials. These solutions don't always come with extra costs. In fact, research from a Unitaid report last year demonstrated for the first time that up to 40% of emissions from health products could be abated without increasing production costs.
A Blueprint for "Climate-Smart Medicines"
By incorporating measures to reduce carbon emissions from the outset of health research and development and optimizing the manufacturing of existing products, the health-care sector can significantly lower its environmental footprint while saving lives. This approach demonstrates that sustainable practices and health advancements can go hand in hand, reinforcing each other as mutual goals.
Sustainable practices and health advancements can go hand in hand
As the health implications of climate change become more obvious, there has never been a more opportune time to act. Last year's UN Climate Change Conference, COP28, adopted a climate and health declaration recognizing the urgent need to integrate health considerations into climate policy. This year's climate conference, COP29, will feature a dedicated health day for the second time, further emphasizing the critical intersection of health and climate.
As scientists, researchers, policymakers, advocates, and people living with HIV conclude the International AIDS Conference in Munich this week, it is time to celebrate the progress made with DTG and to recommit to pushing the boundaries of what's possible in global health. If this magnitude of carbon reduction happened merely by chance, imagine what could be done if the development, production, delivery, and disposal of health products were deliberately designed with the climate in mind, across the entire global health architecture.













