In 1989, an article in the British Medical Journal said "AIDS" on a death certificate was "the final stigma." Fear shrouded hospital wards where previously healthy young people were afflicted with AIDS-related cancers and infections that could quickly take their lives.
Thirty years later, a person diagnosed with HIV at age 20 can now expect to live about 53 more years—a significant health achievement. But more than 800,000 people still die each year due to HIV. Appropriate policy and targeted funding for treatment programs can continue to help reduce HIV deaths. But making policy and funding decisions requires good data.
In 1989, "AIDS" on a death certificate was "the final stigma"
Accurate Death Certificates Influence Health Policy
This is where death certificates come in, and why their accuracy matters. A new study of 132 countries showed that between 1990 and 2018, actual deaths from HIV/AIDS were more than three times greater on average than what was being reported. Death certificates are critical for epidemiologists and policymakers to understand diseases like HIV. Countries with vital registration systems collect their own statistics and researchers analyze this information to identify trends. To measure how well a policy worked, form new ones, or monitor an epidemic, understanding such data on deaths is essential. Without death data, we do not know how many people are dying, when they are dying, and the cause of death.
The debunked accusations of overcounting COVID-19 deaths in U.S. hospitals and data showing COVID-19 deaths in some countries were possibly more than 10 times higher than reported revived interest in death data. Revelations about how COVID-19 deaths are recorded shows how complicated it can be to get it right. Assigning the correct cause of death for COVID-19 requires knowing that the person was positive for the virus and understanding how to record the person's other health conditions—all of which take clinical judgement.
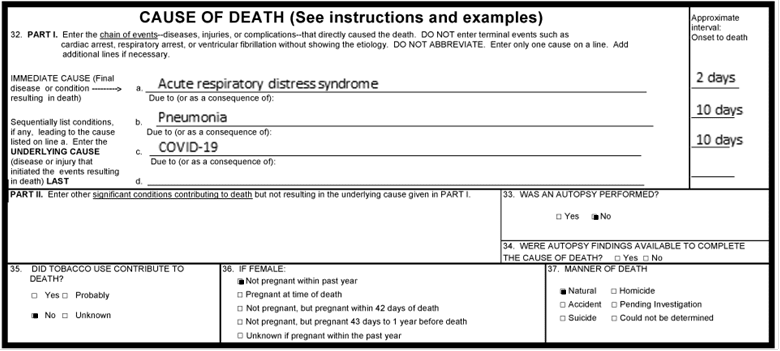
The implications of inaccurate records are profound. For example, for individuals in the United States, pandemic relief funds can be denied if COVID-19 is not on a death certificate despite belief that it should have been, causing further turmoil for grieving families. For society, miscounting can paint a gravely inaccurate picture of an epidemic. Discrepancies between witnesses on the ground and official statistics—vast undercounting—leaves the coordination of resource planning impossible.
HIV: Why Deaths Go Uncounted
For recording HIV/AIDS deaths, the problems with accuracy run even deeper than they do for COVID-19. HIV/AIDS is the underlying cause of death when a person with HIV dies from a condition caused by HIV infection. Historically, doctors have described not reporting HIV/AIDS as the underlying cause of death when there may be severe implications—when patient confidentiality is on the line. Death certificates are public record and listing the cause of death as HIV/AIDS could imply sexual orientation or behaviors that patients do not want disclosed. Patients may also have chosen not to be tested for HIV for fear of losing health benefits.
Percent of Total HIV Deaths in 121 Countries
There are two types of problems embedded in HIV/AIDS deaths reporting that affect the quality of death certificates, and that require different solutions. The first is the need for training and knowledge—an overlooked issue. Some physicians or trainees issuing death certificates simply do not know how to fill out the certificate properly, or do not know enough about the disease. Appropriate training and education can dramatically decrease error rates on death certificates and help to standardize the clinical skills required to fill out death certificates.
The second problem is intentional miscoding, which is driven by stigma and negative consequences. Ensuring that there will be no legal implications, such as lack of insurance coverage and refusal to embalm, will help to encourage truthful certifications. However, stigma is difficult to address. Balancing the individual need for patient confidentiality with the broader need for accurate data is not trivial, but the desire for privacy stems from fear that people living with HIV should not have to face to begin with.
More accurate death data will lead to understanding how many people are still dying of HIV/AIDS—deaths that should now be almost entirely preventable. In addition to the quality issues affecting all death certificates, accuracy remains hindered by the way society still sees those who have the disease. Efforts to ensure appropriate training, and make truthful reporting free of negative consequences, will ultimately result in more accurate data that will allow policymakers and advocates to act effectively.

EDITOR'S NOTE: At the time of writing, the author was employed by the University of Washington's Institute for Health Metrics and Evaluation (IHME) which leads the Global Burden of Disease study described in this article. IHME collaborates with the Council on Foreign Relations on Think Global Health. All statements and views expressed in this article are solely those of the individual author and are not necessarily shared by their institution.












