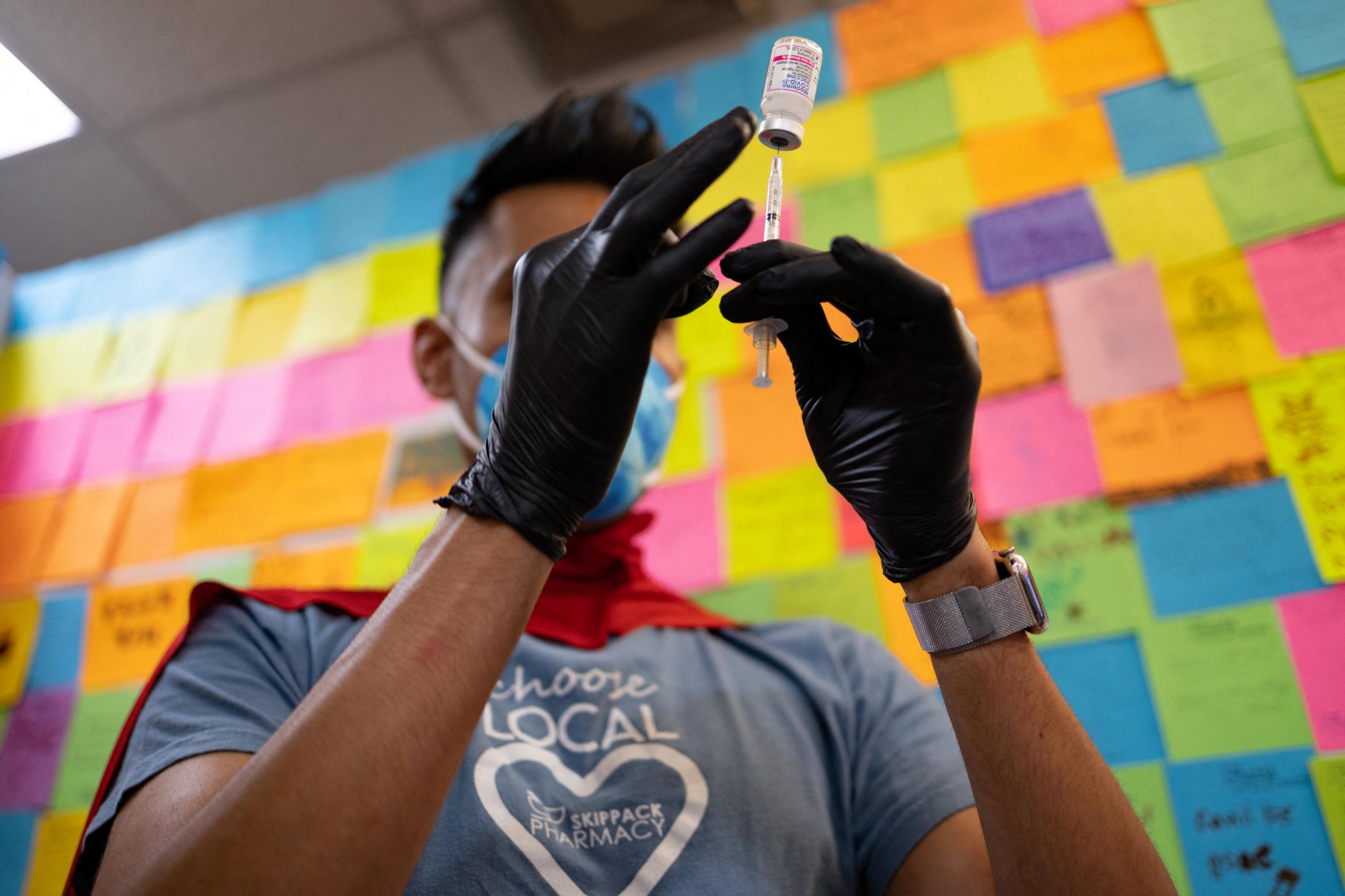
This week, COVID-19 received a little more attention from the public than it's been getting lately when U.S. President Joe Biden announced he tested positive for the virus. Double vaccinated and double boosted, his symptoms are mild and he's working in isolation until he tests negative.
We thought it was a perfect time to turn again to our Institute for Health Metrics and Evaluation (IHME) colleague Ali H. Mokdad for answers to our current COVID-19 questions about the pandemic's wiliest variant yet, omicron BA.5. The chief strategy officer for population health at the University of Washington in Seattle, and professor of health metrics sciences at IHME, shared insights on infection trends, and the current state of testing and tracking.
□ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □
Think Global Health: Dr. Mokdad, thank you for sitting down with us again to talk about where things are with COVID-19. Tell us about the latest subvariant BA.5.
Ali Mokdad: So, what's happening right now is, we have a new omicron variant BA.5 that's circulating. It has two characteristics; one of them is immune escape and it is a super spreader. It spreads much faster than previous variants and is resistant to vaccines, and previous infections do not provide much immunity against it. The vaccines are still highly effective against hospitalization and mortality from BA.5, but they are less effective against it in terms of infection.
Omicron BA.5 makes up about 80 percent of what's circulating now in the United States
Think Global Health: What about people who have had COVID-19? Do they have some natural protection against BA.5?
Ali Mokdad: BA.5 also has immune escape against previous infection, so people who have been infected before by another variant, or even by an omicron variant four or five months ago, are now susceptible and can become infected again because of waning immunity. So, we're seeing a rise in infections right now.
When you look across the United States, it's a wave that's crossing the country. BA.5 makes up about 80 percent of what's circulating in the United States. It has increased so quickly, in a short time, because of these two characteristics of immune escape and waning immunity.
Think Global Health: How are people getting diagnosed with COVID-19 at this point?
Ali Mokdad: Two factors. The first one is that many people are right now counting on home tests to find out if they are infected or not. And some of them are not reporting a positive case, so the reported cases that you look at in the United States right now are basically an undercount. Our estimates are that for every case that is reported there are seven cases out there.
Think Global Health: In the United States specifically, or is that a global estimate?
Ali Mokdad: This is in the United States, and the infection detection rates vary by county. Many locations are not reporting on a regular basis, so we see data dumps in one day and that has reduced our ability to monitor trends in real time and see what's happening.
Think Global Health: In the United States, are states keeping up with case counts, or does the speed at which this subvariant spreads make that difficult?
Ali Mokdad: We're not able right now to know the epidemiology in real time. It takes us one week to look backward and find out what has happened, and that has been a problem. During an epidemic, or a pandemic, you want to know immediately if cases are increasing or decreasing and you want to be able to respond based on how the virus is behaving. Right now, our intelligence and knowledge about this virus is delayed. Our actions are delayed so, for example, by the time we knew about BA.5, it was already spreading so fast in the United States—it had already taken hold.
But if we knew ahead of time that we're seeing a rise in cases and we're seeing a shift, then we could share the trends and the fact that we have a new variant with public health authorities, and they could take proper measures.
Think Global Health: Let's go back to the concept of immune escape.
Ali Mokdad: It means the virus is escaping the protection of the vaccine, which is our best tool. You get the vaccine and you protect yourself, meaning if you get infected, you should be immune against the virus. But what we are seeing right now is people who have been vaccinated and/or have been infected by a previous variant are getting infected right now. And unless you explain to the public that reinfections are happening, it's dangerous. People who've had COVID-19 will think, "Why should I wear a mask? Why should I get my booster? My previous infection is my booster. I should be fine."
Think Global Health: Are we all susceptible to waning immunity?
Ali Mokdad: It's very important for the public to understand waning immunity. COVID vaccines and infections do not provide long-term protection against this virus. If you get a measles vaccine, you will be set up for life. You may need a booster when you're a little bit older, but you're set for life—protected. It's not the case with the COVID virus. Even if you get the vaccine, it only has a five to six month effectiveness.
Think Global Health: And that goes back to this being a wily little virus that keeps reinventing itself basically?
Ali Mokdad: Correct, this virus is mutating, changing. Viruses mutate and we as humans have to adapt to it and change, and if we delay that change, we are going to pay for it. It's like playing a chess game. An opponent makes a move, and you have to change your strategy based on their move.
What we are doing right now in the United States—in many places in this country—people are using exactly the same strategy and that's not the right approach. What has happened here in the United States has been really frustrating. The CDC and the White House are not paying attention to what's happening elsewhere in other countries. They're basing their decisions on the U.S. and the U.S. only.
For me, somebody who monitors what's happening all over the world, I've been watching the omicron BA.5 uptick in Europe. In France, infections went up and almost reached a level of the second wave. In England, cases started going up, in Israel, in Greece—all of the European countries. And here in the United States, we saw it coming and we didn't change our messaging. That's a failure in my opinion. We are not living by ourselves on this planet.
Think Global Health: With flu, every year, we see it make its way to us across the world and land in the United States by fall and winter. Similar pattern every year. Why don't we see that with COVID-19?
Ali Mokdad: Flu is seasonal. We can look at what's circulating in other countries and then we design our vaccine based on what we see circulating and what has circulated in the United States in the previous year.
But COVID-19 is behaving more like pneumonia, not like a flu. Pneumonia doesn't disappear in summer. And this goes back to the issue of waning immunity of the virus. You see two peaks every six months—and depending on the variant, it could be a short or a large wave.
BA.5 has increased so quickly, in a short time, because of two characteristics, immune escape and waning immunity
Think Global Health: What is the "Centaurus" subvariant we're hearing about lately? (A Twitter user nicknamed omicron subvariant BA.2.75 "Centaurus," but the World Health Organization hasn't given it an official name.)
Ali Mokdad: This is the variant of the biggest concern right now. It was detected in India in July and is found in some U.S. states. What we see now is that it is not spreading as fast as BA.5. The two main questions to monitor in the days ahead: can it compete with BA.5 and take over and is it more severe with the immune escape characteristics. With new variants such as this, we look at the infection and mortality rates.
Think Global Health: Do antiviral drugs work well for people infected with the newest subvariants?
Ali Mokdad: They are very important right now. Antivirals save lives and prevent hospitalization. I know personally people who got over COVID in no time because they were able to go to a pharmacy and get the antiviral. But we also do see people who've had a rebound once they stopped the antiviral. The virus isn't knocked out totally and it multiplies and comes back again.

Think Global Health: Speaking of hospitals, what are admissions looking like in the United States and globally, according to IHME's data?
Ali Mokdad: Hospital admissions are increasing right now, in part because of admissions of people who are coming in for things other than COVID but are testing positive for it because now hospitals are doing more testing in the United States. COVID infection is increasing in all ages, but the largest increases are in the elderly.
Our hospitals stopped testing for COVID for outpatient visits, but for inpatients, if you're admitted into our hospitals, you have to be tested.
Think Global Health: Globally speaking, what is happening with COVID? And specifically, how is Africa doing?
Ali Mokdad: Global mobility levels are high and mask use is at the lowest level. With the spread of BA.5, we see a surge in many parts of the world, including Latin America, North America, Europe, North Africa and in the Middle East, Southeast Asia, and Oceania. Countries such as South Africa, Portugal, and Malta that had earlier BA.5 surges suggest these [other countries currently seeing surges] will peak after four to six weeks. We expect the same here in the United States.
In Africa right now, we don't see large infection waves, and we are not seeing a big surge of cases and that's a big question mark. Why? The surveillance systems are not adequate and part of it may, unfortunately, be due to a previously high infection rate. We are seeing a rise in countries where there is tourism due to people interacting—indoors, in restaurants and bars.
Think Global Health: What do we know about long COVID at this point in the pandemic?
Ali Mokdad: We are concerned about it. It's very common—about 15 percent right now among people who get COVID. And its scope depends on the person. But we even see it in young people who have never had any health problems. People lose their hair, lose memory, feel tired, and some people will still have headaches every now and then. It is different for different people. But it is a reality and calls for all of us to protect ourselves.
Think Global Health: Any final advice about COVID-19 right now?
Ali Mokdad: Even if you get over COVID, or if you had minor symptoms, you need to be very careful and make sure that you don't get it again.