The COVID-19 pandemic, now entering its third year, has resulted in over 445 million confirmed cases of disease and has killed six million people worldwide. By December 2021, more Americans had died from COVID-19 than during the 1918 Flu Pandemic. The decline in life expectancy in the United States between 2018 and 2020 represents the largest drop since World War II. Multiple factors have influenced the number of deaths caused by COVID-19, including the development and distribution of vaccines and antiviral therapies, innovations in health care, mask-usage, and social distancing. However, survival rates also depend on the population's general health, which depends in part on long-term health-care trends. This begs the question: How did pre-pandemic health-care trends impact COVID-19 mortality rates?
Health-care Innovations and Improvements in Comorbidity Control
The most common risk factors associated with worse COVID-19 outcomes are older age, male sex, and comorbidities including diabetes, hypertension, and cardiovascular disease. The prevalence of several of these risk factors has increased in recent decades. The U.S. adult population aged 65 and older increased by 58 percent, from 31 million in 1990 to 50 million in 2017. Worsening trends in diet, body weight, and activity also led to an increase in diabetes prevalence among those 65 and older, from 10 percent in 1990 to 19 percent in 2017.
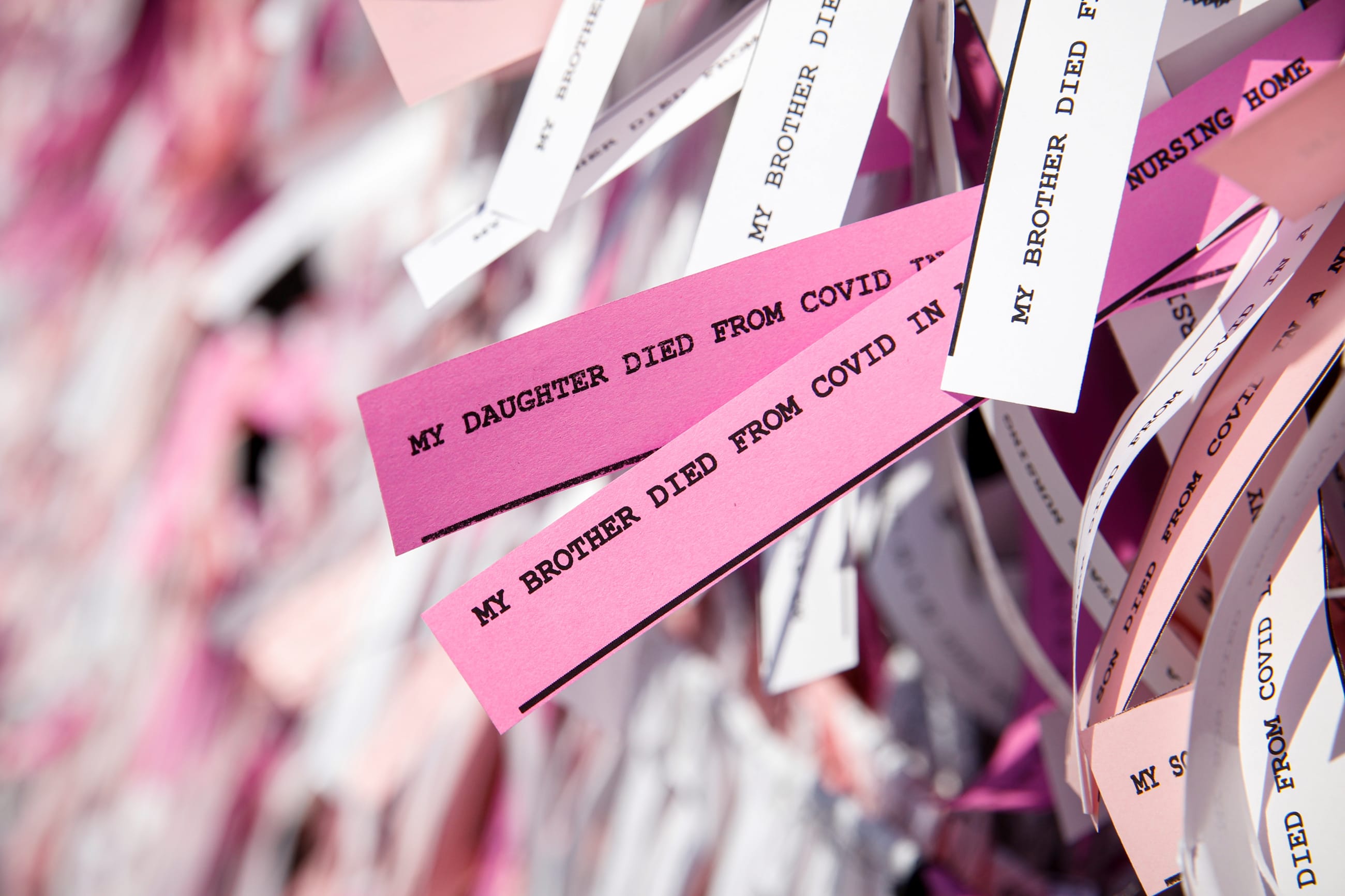
By December 2021, more Americans had died during the COVID-19 pandemic than during the 1918 influenza pandemic
On the flipside, health-care innovations introduced in recent decades have improved control of COVID-19-related risk factors. For people with diabetes, continuous glucose monitoring devices can facilitate rapid treatment decisions and reduce acute diabetes-related complications, leading to improved health outcomes. The rate of good glycemic control – a measure of diabetes management – has increased substantially, from about 40 percent in 1988 to an estimated 72 percent in 2017. Similarly, people with hypertension and cardiovascular disease have benefitted from new drugs including angiotensin-converting-enzyme (ACE) inhibitors and statins. The rate of controlled hypertension increased from 32 percent in 1999 to 48 percent in 2016. Perhaps because of better management of these conditions, the prevalence of cardiovascular disease decreased by about 5 percent between 1997 and 2016. Advances in disease management prompt a natural question: How much worse could the COVID-19 pandemic have been in the United States if the burden of these comorbidities had not declined?
What are the COVID-Related Benefits of Improvements in Comorbidity Control?
We developed an open source model to explore how health-care innovations for diabetes, hypertension, and cardiovascular disease could have affected the number of COVID-19-related hospitalizations and deaths among individuals age 65 and older during the first wave of the pandemic (March-July 2020). The model assumes that 1.4 percent of individuals in this age group with any of these comorbidities becomes hospitalized, based on data collected during the pandemic's first wave. For those hospitalized, mortality risk depends on gender, age stratification (age 65-74 vs. age 75 or older), comorbidity (diabetes, hypertension, or heart disease), and, for cases of hypertension and diabetes, whether the condition is well-controlled. We assumed that better control would not eliminate mortality risk entirely; rather, improvements in control would reduce COVID-19 mortality risk by 45 percent, consistent with published reports of the benefits of comorbidity control.
Mortality Reduction from Improved Treatment of COVID-19 Risk Factors
Using the model, we developed a scenario using the 2017 age and gender distribution, the 2017 prevalence rates for diabetes and hypertension, and the 2017 proportion of diabetes and hypertension patients with well-controlled vs. poorly controlled disease. Our comparator scenario assumes that for diabetes and hypertension, the proportions of patients with well-controlled disease remain at their less favorable 1990 levels while holding population estimates constant at 2017 levels. Under these assumptions, the 2017 control rates, which improved for diabetes and hypertension, reduced the estimated number of COVID-19 deaths among elderly hospitalized patients in the United States by about 12 percent, from 104,000 estimated deaths using the 1990 control rate to 92,000 deaths using the 2017 control rate.
For cardiovascular disease, we used 2016 population data for assumptions about the number of individuals over the age of 65 in both scenarios, but we used different assumptions for the cardiovascular disease prevalence rate, with one scenario using the 2016 rate (23 percent for adults age 65-74; 37 percent for 75 and older) and the comparator scenario using the higher 1990 rate (28 percent for adults age 65-74; 37 percent for 75 and older). We did not characterize the degree of control for this comorbidity, as there is no widely accepted criterion and tracking for this characteristic. With population held constant at 2016 levels, the estimated number of COVID-19 deaths decreased by 8 percent, from 67,000 deaths, when using 1990 cardiovascular disease prevalence, to 62,000 deaths when using 2016 prevalence.
Comorbidity control and prevalence reduction prevented more than 25,000 deaths during the first wave of the pandemic
Among individuals with any of the three comorbidities, our estimate for the number of COVID-19 fatalities among individuals age 65 and older decreased from 171,000 using the 1990 prevalence and control rates to 154,000 using the corresponding 2017 rates. This result implies that comorbidity control and prevalence reduction prevented about 17,000 deaths during the first wave of the pandemic.
Our model can answer other questions, too. For example, how many COVID-19 deaths among individuals age 65 and older with diabetes were averted by improvements in diabetes control between 1990 and 2017? (Answer: 4,900). Or, by how much does the expected number of COVID-19 deaths decrease for individuals age 65 and older with hypertension if we assume that comorbidity control reduces mortality risk by 80 percent, rather than by our primary assumption of 45 percent? (Answer: 12,000). This analysis highlights the extent to which innovation in recent decades for other diseases may have helped to reduce COVID-19 mortality.
Downstream Benefits of Investments in Health-Care Innovation and Lessons for Future Pandemics
Is the suggestion that about 17,000 lives were saved over approximately three months substantial? Between 2010-2011 and 2019-2020, the United States averaged around 34,000 flu deaths annually. The National Institutes of Health estimates that between January and May, 2021, the introduction of COVID-19 vaccines prevented 265,000 COVID-19 infections, 107,000 hospitalizations, and 39,000 COVID-19 deaths among Medicare beneficiaries. The estimated prevention of 17,000 COVID-19-related deaths in the same age group during the first wave of the pandemic is in this ballpark. Of course, unlike vaccines, better control of diabetes and hypertension, and a reduction in the prevalence of cardiovascular disease do not come with the prospect of ending a pandemic. But in the context of lives saved during a pandemic – these advances highlight how innovations to improve the population's overall health have downstream benefits when a national health emergency— like COVID-19— arises.
What Does this Mean for Global Health?
While the analysis focused on a high-income country with reasonable access to medicines and other health services that can help control comorbidities, diabetes and hypertension are also major concerns in low- and middle-income countries (LMICs). There, challenges in access to health care, health services, and financing mean that the need for prevention and treatment of non-communicable diseases goes largely unmet. As part of preparedness for future pandemics, organizations that support health system strengthening in LMICs have a responsibility to support improvements in the baseline health of the population, too. As observed in these findings, decades of investment in treatment for diabetes, hypertension, and heart disease have had a positive downstream benefit in COVID-19 mortality rates and have prevented an already devastating pandemic from becoming worse. With the COVID-19 pandemic moving to the endemic stage, and with continuing challenges in encouraging people to wear masks, socially distance, and get vaccinated, this model underscores the value of investing in, developing, and increasing access to innovative medical treatments that can better control chronic conditions and mitigate the effects of future pandemics.

AUTHORS' NOTE: The authors are employed by Tufts Medical Center. Development of the model was funded through an unrestricted grant from Amgen, Inc. Neither our employer nor the funder were involved in the development of the model, and neither entity had editorial control over the contents of the proposed blog, which was managed entirely by the authors.