While COVID-19 is a fast-moving crisis that is exploiting countries' vulnerabilities, there is another health crisis that has been smoldering for decades, wreaking havoc on the world—resistance to antibiotics. These medicines have been increasingly losing their potency due to overuse. Illnesses that used to be largely curable, such as tuberculosis, blood infections, and pneumonia, have become fatal. In the most dire projections, medicine as we know it could become a distant memory as our ability to perform surgery, give chemotherapy, and ensure safe hospital stays is compromised by infections that can no longer be treated or prevented by antibiotics.
A new study of antibiotic resistance has uncovered its global burden. Already, the burden of antibiotic resistance is larger than that of HIV/AIDS and malaria, causing over 1.2 million deaths in 2019. These include deaths that would have been prevented if bacteria hadn't become resistant to antibiotics.
The burden of antibiotic resistance is larger than that of HIV/AIDS and malaria
The true death toll of antibiotic resistance is likely even larger. The study found that antibiotic resistance was associated with more than 4.9 million deaths in 2019, meaning that antibiotic resistance contributed to death, but wasn't necessarily the direct cause. (The 4.9 million deaths included the more than 1.2 million deaths that were directly caused by antibiotic resistance).
This study leverages hospital and laboratory data from around the world as well as data from published studies. Members of the Institute for Health Metrics and Evaluation-led Global Burden of Disease Network, which includes more than 7,000 collaborators in 157 countries and territories, collaborated on the study and provided data.
Where Antibiotic Resistance Is Deadliest
The study found that the largest burden of antibiotic resistance in the world occurs in sub-Saharan Africa and South Asia, and the regions with the lowest burden are East Asia, North Africa and the Middle East, and Australasia (including Australia and New Zealand). Surprisingly, the high burden of resistance in sub-Saharan Africa is seen despite antibiotic use being lower than it is in high-income countries and resistance to antibiotics being less common; rates of infectious diseases are so high in sub-Saharan Africa that the sheer number of infections in the region translates into a greater burden from antibiotic-resistant infections. This is compounded by insufficient local access to second-line antibiotics (such as cefepime)—the type of antibiotics that health-care workers use to treat infections when other more common antibiotics (such as penicillin) fail to work. Low-level antibiotic resistance that would be easily treated in high-income countries is incurable without access to these second-line medications. A lack of access to lifesaving medications may be a major driver of the burden of resistance in sub-Saharan Africa.
Deaths per 100,000 Attributable to Antibiotic Resistance, in 2019
The different factors that drive resistance to antibiotics are complex and can vary from location to location. For example, in high-income countries, overuse of antibiotics has contributed to much of the resistance. In contrast, in areas of sub-Saharan Africa, the rate of antibiotic use is substantially lower and resistance is driven, at least in part, by a lack of access to clean water and sanitation. To tackle antibiotic resistance, approaches tailored to each location are vital.
Stifling the Threat of Antibiotic Resistance
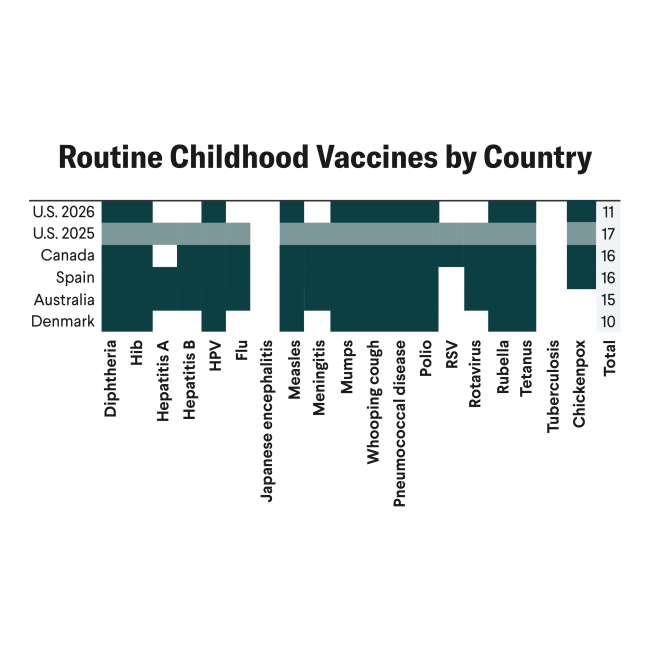
There are a variety of proven interventions that leaders can use to curb this growing threat to people's health. For example, developing new vaccines to prevent common infections drives down the need for antibiotics, which in turn reduces antibiotic resistance. Of the six major infections that account for the bulk of the lives lost to antibiotic resistance, there is only one vaccine that exists today—the pneumococcal vaccine for Streptococcus pneumoniae (a bacteria that causes pneumonia and meningitis). But new vaccine programs are underway for Staphylococcus aureus (staph), Escherichia coli (E. Coli), and other infections that contribute to much of the disease burden. Greater investment and urgency is needed, however, and even a fraction of the success we witnessed in the development of COVID-19 vaccines could prove lifesaving.
Overcoming challenges to get vaccines into arms is equally important—another lesson learned from efforts to vaccinate the world against COVID-19. Investments in boosting health systems' capacity to deliver vaccines and ensuring ample, predictable, and reliable supplies of vaccines are also critical. In addition to developing and delivering new vaccines, the world needs to bolster the pipeline for new antibiotics, and make sure second-line antibiotics are accessible to anyone who needs them. Funding for these efforts has been minimal, and most of the major pharmaceutical companies have stopped investing in research and development for antibiotics due to lack of profitability.
Deaths per 100,000 Attributable to Antibiotic Resistance by Region, in 2019
Hygiene, Clean Water, and Sanitation
While the drug development pipeline is a critical component to combatting resistance, it would be only a matter of time before resistance develops to any new drugs without investment in programs to optimize their use and slow the spread of resistance. These include programs that improve access to clean water, sanitation, and hygiene, as well as infection prevention and control programs in health facilities. For instance, in health facilities, installing hand sanitizer dispensers next to each hospital bed can reduce the likelihood of antibiotic-resistant infections spreading from person to person. And in communities, especially in settings without widespread access to safe water and sanitation facilities, expanding access decreases infections, lowering the need for antibiotics.
The Right Antibiotic for the Right Infection
Optimizing antibiotic use plays a large role in combatting resistance, too. Antibiotics are vital to curing many bacterial infections, and it's essential that effective antibiotics are available when needed, but the right antibiotic needs to be used for the right infection. In a similar vein, when the culprit is a virus instead of a bacteria, antibiotics are not useful. Appropriate prescribing can only be achieved if health care providers are able to run tests to accurately diagnose and treat these conditions. So, having testing equipment and laboratory infrastructure is key. Unfortunately, accessing these essential tools is a challenge in many low-resource settings.
Curbing the routine use of antibiotics in livestock may also be an effective strategy to combat antibiotic resistance, research shows. Antibiotics are used to enhance production of meat in many countries because they can increase growth, protect against disease, and lower costs. Antibiotic resistance evolves slowly, and its insidious spread can lead to complacency even though resistance could ultimately end up killing even more people than this pandemic has to date. Like COVID-19, antibiotic resistance knows no borders, and the global spread of highly antibiotic-resistant bacteria has been well documented. If we internalize lessons from what has gone wrong with COVID-19, addressing this crisis as a global community before it's too late, we will benefit all.
ACKNOWLEDGEMENTS: The authors would like to thank Rebecca Sirull for fact-checking assistance, Eve Wool for logistical support, and Catherine Bisignano and Connie Kim for providing feedback.
EDITOR'S NOTE: The authors are employed by the University of Washington's Institute for Health Metrics and Evaluation (IHME), which leads the Global Burden of Disease study described in this article. IHME collaborates with the Council on Foreign Relations on Think Global Health. All statements and views expressed in this article are solely those of the individual authors and are not necessarily shared by their institution.