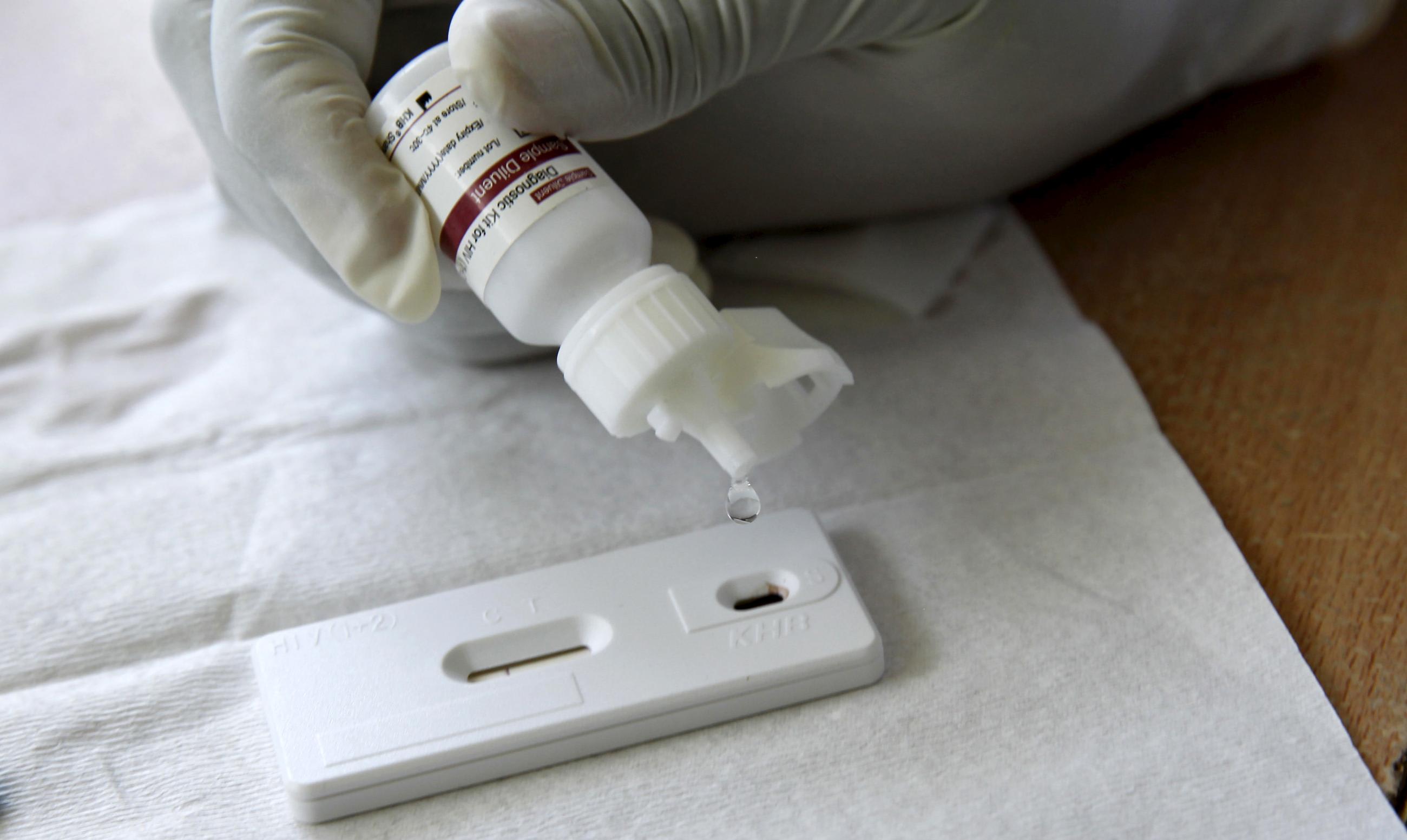
In late 2022 in Malawi, the District Health Office (DHO) coordinator for sexually transmitted infections (STIs) noted an issue in Blantyre, the country's HIV prevention data dashboard known as the Prevention Adaptive Learning and Management System, or PALMS. Cases of STIs had spiked around a public health facility but no comparable increase in HIV testing or initiation onto pre-exposure prophylaxis (PrEP) was evident.
Knowing that STIs can be a leading indicator of HIV infections, the DHO coordinator notified her colleagues, launched a data review meeting, investigated the issues at the facility and community levels, and supported the facility to react and blunt what could have been a surge of HIV infections.
Three years ago, it would have been almost impossible to spur such action. A coordinator would have lacked access to all of the data and training to interpret it, and the local HIV prevention ecosystem lacked the tools and resources to respond rapidly or cohesively.
Three years ago, it would have been almost impossible to spur such action
Decentralization processes in many countries require DHOs, provinces, counties, and other local entities to take on more of the planning, resource allocation, implementation, and coordination of public health efforts. However, they often lack the coherent systems needed to lead effective HIV prevention responses.
The Blantyre Prevention Strategy (BPS), a government-led partnership launched in May 2020, has worked to address those gaps in Malawi's second largest district by elevating local leadership, increasing access and capacity to use data, and strengthening partnerships among communities, service providers, and the government.
BPS is organized around a central truth about the path to greater sustainability—that the combination of support for subnational leadership, development of core public health functions, and multisectoral coordination has great potential to expand the effectiveness and sustainability of health systems. By developing the technical, governance, and stakeholder engagement capabilities and capacities of the district and city health teams, as well as facilities and other key local actors, BPS provides an example of how it is possible to foster a system capable of detecting and targeting disease risks, generating demand for HIV prevention services, effectively delivering prevention products and interventions, and supporting sustained use of prevention products. It is transforming HIV prevention into a nimbler, data-forward system that grows the capabilities of subnational health systems under local leadership, enables community participation, and supports integration with functions of global health response.

Yet the vital role that subnational governance and systems development play in sustainable public health is generally not prioritized within global HIV strategies or investments. Exceptions include the UNAIDS HIV 2025 Prevention Roadmap, which recognizes an imperative to "strengthen national and subnational entities responsible for overseeing implementation of HIV prevention programmes, including those outside the public health sector." What is often missing in the global guidance, however, is the how or by whom or even the why, not to mention a call for associated financial investment in building oversight capacities at subnational level.
BPS demonstrates some of the how and why investing in a subnational system can contribute to sustainability. When the Ministry of Health, National AIDS Commission, and I now join the DHO coordinators and facility staff in Blantyre, we see example after example of how they are working together within a cohesive, government-led system. They routinely access data in PALMS, which links and presents HIV and related data in user-friendly dashboards. The system flags assist with passive surveillance of HIV infections. The coordinators also work with facilities and community health workers to understand hotspots and coordinate response activities.
The DHO coordinators run community labs to gather insights from clients and communities that are informing demand generation activities and improvements to service delivery—as well as national policies. They provide quality improvement mentorship to facilities on the provision of PrEP and promote sharing across facilities and partners. They are building linked networks with facilities, political leaders, and community and partner organizations to address service gaps and structural drivers of HIV infection collaboratively.
They are building linked networks with facilities, political leaders, and community and partner organizations
By strengthening the system, BPS has created paths for high-impact, subnational donor and government investment. The Ministry of Health's recognition of the effectiveness of systems change in Blantyre has led to elements of the project being adapted to the next largest district in Malawi, where it will strengthen the rollout of long-acting injectable HIV PrEP.
Malawi is not alone in putting local governments in a central role on HIV. In India, decentralization of the national AIDS control program has allowed states and districts to steer implementation according to local needs. In Kerala state, that has led to innovative strategies to assess community risks and provide outreach to key populations, such as targeted programs among female sex workers and men having sex with men in Malappuram district.
Yet few examples exist elsewhere of investments in strengthening government-led systems specific to HIV prevention at subnational level. Momentum needs to be built to make a concerted shift toward funding subnational systems as an essential component of achieving a sustainable response and ending HIV as a public health threat by 2030.

Encouragingly, in October 2022, the Finance in Common Summit called for development banks and a broadline coalition of donors to create an investment agenda to build "institutional, human, and physical capital for health services" in local institutions at both national and subnational levels. Likewise, on World AIDS Day in 2022, the U.S. President's Emergency Plan for AIDS Relief (PEPFAR) released a five-year strategy, Fulfilling America's Promise to End the HIV/AIDS Pandemic by 2030, emphasizing "Sustaining the Response" as one of its five strategic pillars.
The strategy includes development of country-led sustainability plans. In September 2023, PEPFAR convened country representatives, multilateral organizations, and civil society to begin a year-long process to develop sustainability roadmaps with the goal of completion by World AIDS Day 2024.
This movement is important but will require thoughtful engagement at country level. Local officials need to be front and center of sustainability planning with associated investment in the capabilities needed for effective on-the-ground responses. Prioritizing subnational models of leadership in the development of these roadmaps will support countries' decentralization goals and create stronger platforms for sustainability.