Poor diets produce staggering health damage and social and economic costs globally. Health systems in the United States and other countries have not adequately addressed diet-related diseases, nutrition deficiencies, and the health disparities those diseases and deficiencies exacerbate. New interest in Food is Medicine strategies is stimulating meaningful action that enhances the synergies between nutrition and disease treatment and prevention in health systems. These strategies have potential to improve health outcomes and equities in the United States and around the world.
The Scourge of Diet-Related Diseases
Diet-related chronic diseases are the leading cause of human suffering and deaths worldwide—with worsening trends across nations at all income levels. Poor diet is estimated to cause approximately half of the cardiometabolic deaths in the United States, one-third of the world's coronary heart disease deaths, and almost three-fourths of new diabetes cases globally. Across the world, nutritional quality is below recommended guidelines, with average national diet scores of only 30 to 45 out of 100 in all regions.
Diet-related chronic diseases cause serious health disparities by ethnicity, geographic residence, income, and race. These disparities are exacerbated by food insecurity—inadequate or unstable access to enough nutritious food—as well as by education, health-care access, housing opportunities, and lower income. In this way, suboptimal nutrition and food insecurity are major mediators of health inequalities.
Diet-related conditions are also costly. The U.S. economy annually loses an estimated $963 billion in medical expenditures and lost labor productivity from poor nutrition and $146 billion from food insecurity—a total of $1.1 trillion in yearly economic losses.
Individual knowledge or choice alone does not drive population burdens of poor nutrition. Instead, complex agricultural, cultural, economic, environmental, political, and social determinants are involved. When billions of people around the world—including children and young adults—suffer from diet-related illnesses, the system is broken. System problems require system solutions.
When billions of people around the world—including children and young adults—suffer from diet-related illnesses, the system is broken
Importantly, diet-related diseases have two major drivers: excessive intake of harmful factors (such as refined grains, processed meats, sodium, sugary beverages, and trans fats) and inadequate consumption of protective foods (such as fish, fruits, legumes, nuts, plant oils, vegetables, whole grains, and yogurt). Many nations' policies on diet-related diseases focus more on reducing consumption of the harmful factors.
Such harm-reduction strategies mirror tobacco control policies associated with the World Health Organization's Framework Convention on Tobacco Control. Those policies emphasize negative messaging and disincentives through increased taxation, marketing restrictions, and warning labels. Chile, Mexico, and other Latin America nations have launched such approaches in their efforts to counter diet-related diseases.
Those strategies can work against isolated additives, such as sodium, or products with no nutritional value, such as sugary beverages. However, the strategies do little to increase the consumption of minimally processed healthy foods.
Health-System Response
In the United States, the health, equity, and economic impacts of poor diet have prompted calls for the health sector to play a greater role in addressing nutrition. That new direction aligns with health-system transitions toward population health and health equity; new care and payment models that prioritize value-based care and prevention; and growth in digital health information, online food purchasing, and food-delivery systems.
Health systems generally do not address nutrition—the top driver of poor health
Historically, doctors had few practical options to improve patient diets—a problem compounded by inadequate medical nutrition education, electronic nutritional screening or decision support, incentive and reimbursement mechanisms, or team-based care. Accordingly, scalable, effective health-sector interventions to improve nutrition, diet-related diseases, and related disparities have been lacking. The irony is all too real: health systems generally do not address nutrition—the top driver of poor health.
Food Is Medicine
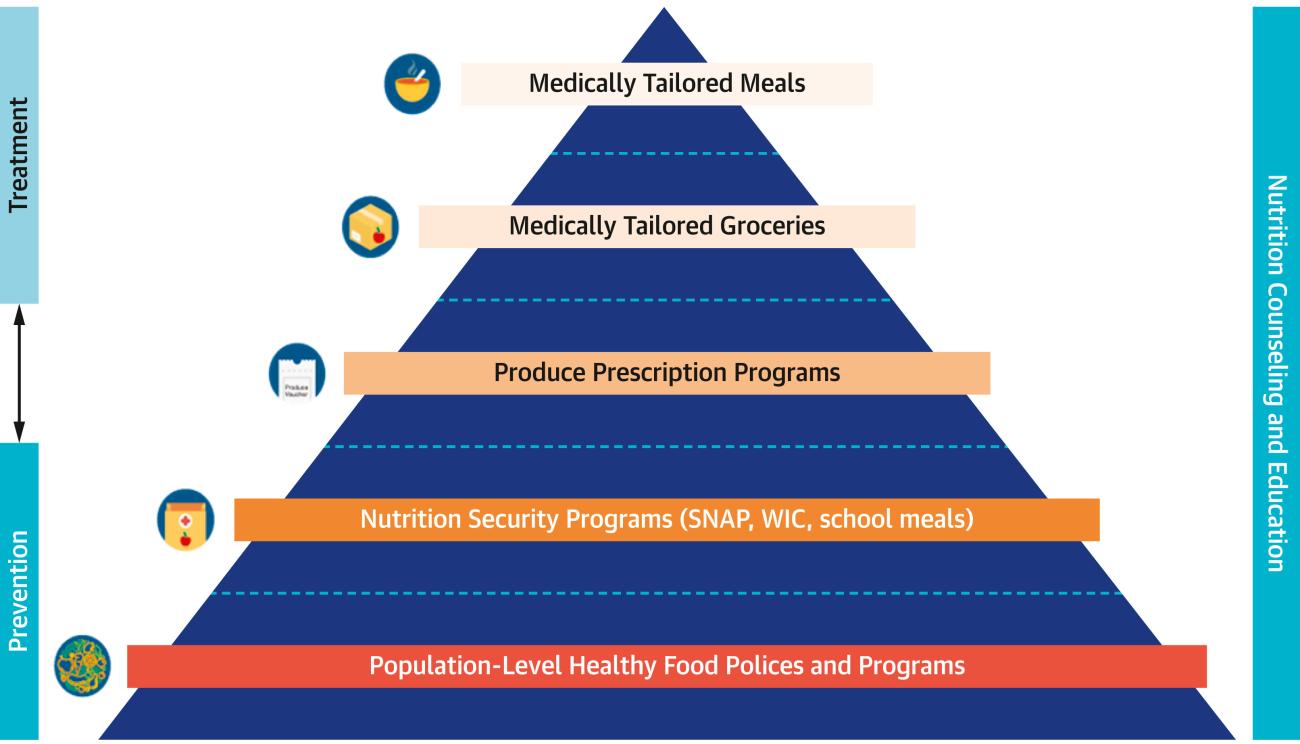
That reality is changing across U.S. health care and policy through new Food is Medicine (FIM) strategies. FIM features a spectrum of food-based nutritional programs, services, and other interventions that are integrated within and support health-care system responses to the critical link between nutrition and health. FIM interventions focus on increasing the access, affordability, availability, and consumption of healthy foods. FIM programs include more intensive meal-based treatments for sicker patients with complex medical conditions, broader grocery-based treatments for patients with common diet-related maladies, and foundational population policies to support healthier eating for all. In short, FIM adds to the policy armamentarium for increasing consumption of healthy foods.
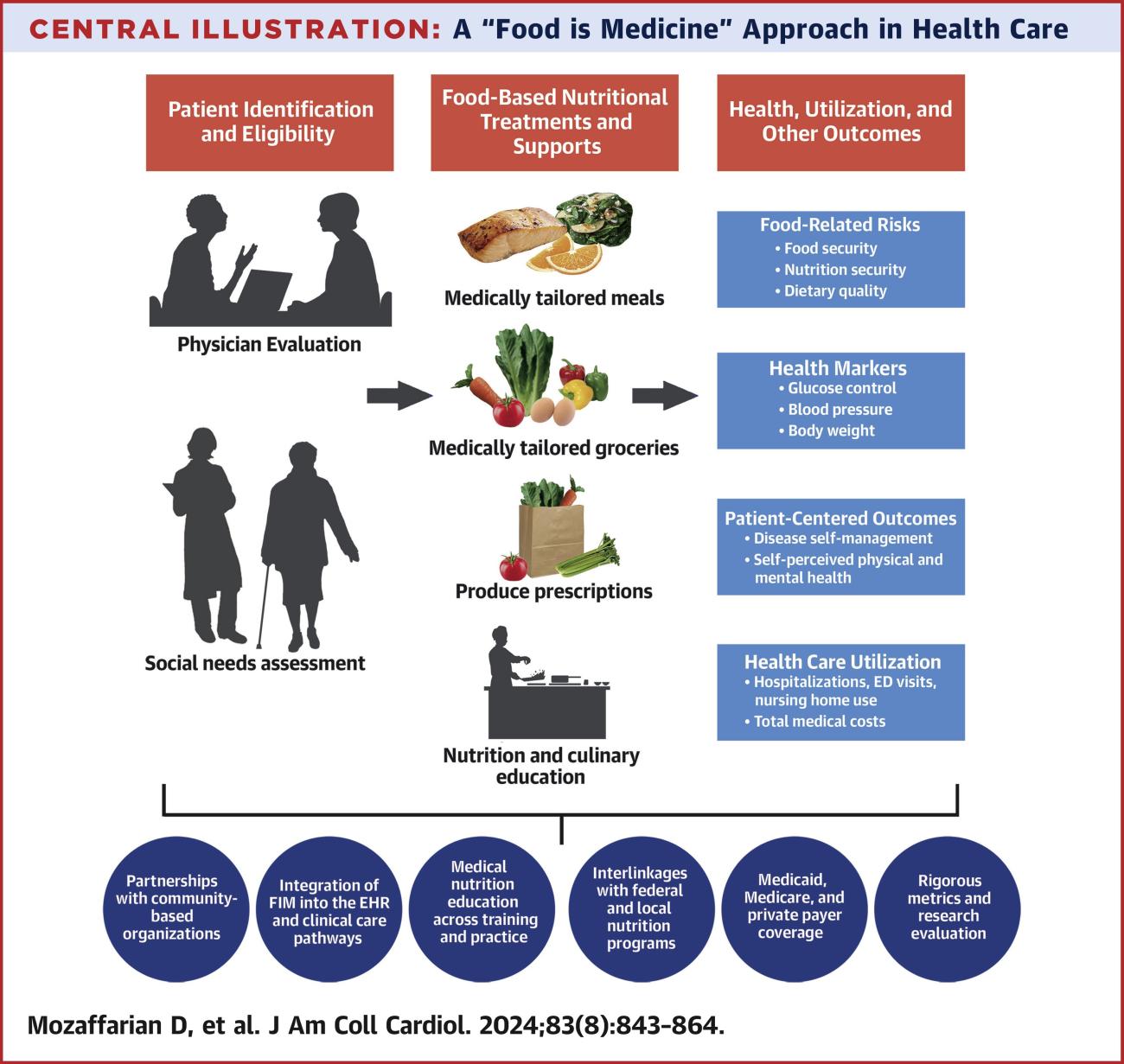
Physicians generally identify eligible patients as those who have at least one diet-sensitive condition and one or more social stressor, such as financial strain, food insecurity, or homelessness. Commonly targeted medical diagnoses include cancer, chronic kidney disease, diabetes, heart failure, high-risk pregnancy, HIV, and hypertension.
Although the preventive benefits of good nutrition are important, FIM interventions typically focus on disease management to treat and reduce complications—a therapeutic approach that can produce return-on-investment within months rather than decades. In this way, FIM functions more like traditional medical treatment than a preventive or social needs intervention. Even so, most FIM programs emphasize population health and health equity by including strategies to reach socially vulnerable patients.
Therapeutic FIM interventions provide medically tailored meals or groceries to eligible patients, partly or fully covered by health insurance. Patients with complex, significant medical needs receive more intensive meal services. Less intensive grocery or produce interventions target larger populations with diet-sensitive conditions or risk factors.
Social workers or community health workers often identify and refer patients; registered dietitian nutritionists provide expertise to tailor the food to medical conditions and patient preferences. Nutrition and culinary education delivered in-person or digitally adds support. Other supportive innovations include electronic health-record screening for food and nutrition security and diet quality; clinical care pathways and payment models to support screening and referral to FIM; and new curricular, accreditation, and licensing efforts for greater nutrition education for doctors.
So far, FIM training of physicians has been variable. National calls are growing to increase nutrition education for doctors, with some initial response from medical and other health professional schools, health-related societies, licensing boards, and accreditation councils.
In addition to reducing food security, FIM interventions address nutrition security—the access, availability, and affordability of foods and beverages that promote well-being and prevent or treat disease. The concept of nutrition security builds on that of food security in aiming to prove both sufficient calories and sufficient nourishment.
The COVID-19 pandemic highlighted the importance of nutrition security. The pandemic exacerbated food insecurity and poor nutrition in vulnerable populations. It also revealed that diet-related chronic conditions (for example, diabetes, hypertension, and obesity) were major drivers of adverse health outcomes and disparities for patients infected with COVID-19.
FIM's Effectiveness
Although studies of the impact of FIM interventions have varied in design, target population, and intervention components, the overall evidence suggests FIM programs improve food security, nutritional quality, health-care utilization, and health outcomes. For example, produce prescriptions increase fruit and vegetable consumption by an average of about 0.8 servings per day and partially replace unhealthy items such as fast foods and salty or sugary snacks. Produce prescriptions also appear to reduce hemoglobin A1c, obesity, and blood-pressure levels by modest yet clinically meaningful amounts.
The pandemic exacerbated food insecurity and poor nutrition in vulnerable populations
More limited assessments suggest that FIM interventions can improve important patient-centered outcomes such as disease management and mental health. Provision of medical meals to high-risk patients with complex chronic conditions appears to reduce emergency department visits, hospitalizations, and total medical costs. In a national simulation model, providing medical meals to the approximately 6.3 million U.S. eligible adults produced an estimated annual net savings (accounting for the intervention's cost) of $13.6 billion. To date, most FIM studies have utilized before-and-after evaluations of interventions. Larger, longer-term, and randomized controlled trials are needed. Several of those trials are under way, including on cancer, diabetes, and high-risk pregnancy.
FIM supports health equity by focusing on vulnerable populations and helping address structural barriers to better nutrition. Often, innovations in clinical medicine do not advance, and can even worsen, health disparities because they are less available and less prescribed to patients who need them most. FIM programs, however, are designed to reach vulnerable populations that have specific medical conditions and are experiencing food insecurity, financial strain, or other social challenges. FIM interventions have the potential to improve health and achieve better health equity.
Shifting National Programs and Policies
As evidence on FIM has grown, interest among health-care payers and policymakers has increased. The major federal health insurance programs increasingly cover FIM services. Eleven U.S. states are testing FIM in Medicaid, the program for low-income Americans. FIM is also being implemented in Medicare, the program for Americans older than 65. In 2020, 101 Medicare Advantage plans covered FIM. By 2023, coverage had increased to 929 plans, demonstrating expanded interest.
The Centers for Medicare and Medicaid Services has released a framework and guidance on how to implement FIM, and the Department of Health and Human Services convened an inaugural FIM Summit in February 2024. Commercial payers are also advancing FIM. Kaiser Permanente has committed $50 million to FIM. Aetna, Blue Cross/Blue Shield, Elevance Health, Geisinger Health, ProMedica, and others are taking action as well. Those public and private initiatives demonstrate broad interest among payers in piloting and scaling up FIM.
Given increased demand, FIM vendors of medically tailored meals or groceries are expanding. These include private-sector companies, such as FarmboxRx, Foodsmart, Instacart Health, Kroger, Mom's Meals, Nourished Rx, Performance Kitchen, Season Health, VitaBowl, and Walmart. Nonprofit community organizations, such as those in the Food is Medicine Coalition and National Produce Prescription Collaborative, are also expanding their FIM efforts.
In medical education, the U.S. House of Representatives recently adopted a bipartisan resolution calling for expanded, substantive nutrition education for doctors. The U.S. accrediting body for medical residencies and fellowships in 2023 announced plans to integrate mandatory nutrition education into all programs by 2026.
The White House accelerated the momentum in 2022 when it convened a conference and released an ambitious National Strategy on Hunger, Nutrition, and Health. The strategy outlined a coordinated national approach to changing policies, programs, and systems at government, private sector, and civil society levels to advance food and nutrition security for the population. FIM is a core pillar of the plan.
Government agencies are also responding. The Centers for Disease Control and Prevention, Department of Agriculture, Department of Veterans Affairs, and Indian Health Service are implementing FIM programs. The Department of Health and Human Services and the National Institutes of Health have established new FIM research goals. A White House-led interagency working group meets regularly to coordinate and advance the federal government's efforts.
Finally, intense demand for, the high cost of, and low long-term adherence to new anti-obesity drugs (GLP-1 agonists) is encouraging payers and providers to test FIM and related approaches, to both reduce the need for those drugs and, among those who use them, support their long-term success.
On the Horizon
The expansion of FIM interventions in the United States has been remarkable, and new policies and programs are rapidly accelerating across the country. In contrast, other nations are only starting to pilot FIM projects. Given the economic, disparity, and health impacts of poor nutrition globally, FIM is one critical solution that every country can use. Research gaps remain, requiring additional rigorous and iterative evaluations.
FIM success will depend on partnerships among academia, civil society, health-care systems, payers, policymakers, and the private sector to evaluate, optimize, and scale promising interventions. Collectively, those strategies can improve nutrition, advance health, prevent diet-related diseases, and lower the economic costs and societal disparities associated with such diseases. It is time for health systems in other nations to take notice.
EDITOR'S NOTE: This article is part of a series exploring global food systems guest-edited by Jack Bobo. The other articles in the series can be found here.


